
DISCECTOMY
A discectomy is a surgical procedure to remove the protruding or
damaged portion of a herniated disk in the spine. Discectomies
are highly effective in treating sciatica, which when the protruding
disc exerts additional pressure on the spinal nerves.
What is a Discectomy?
A discectomy is a surgical procedure to remove the protruding or damaged portion of a herniated disc in the spine. Discectomies are highly effective in treating sciatica, which when the protruding disc exerts additional pressure on the spinal nerves. I am very experienced in this operation. I will discuss all benefits and risks of the procedure with you at your consultation. If you have any concerns about the procedure please ask me during your consultation.
I work with a team of three consultant surgeons, consultant radiologist and a very experienced physiotherapy team and discuss all complex cases in our fortnightly multidisciplinary team meeting to be able to provide a first class service.
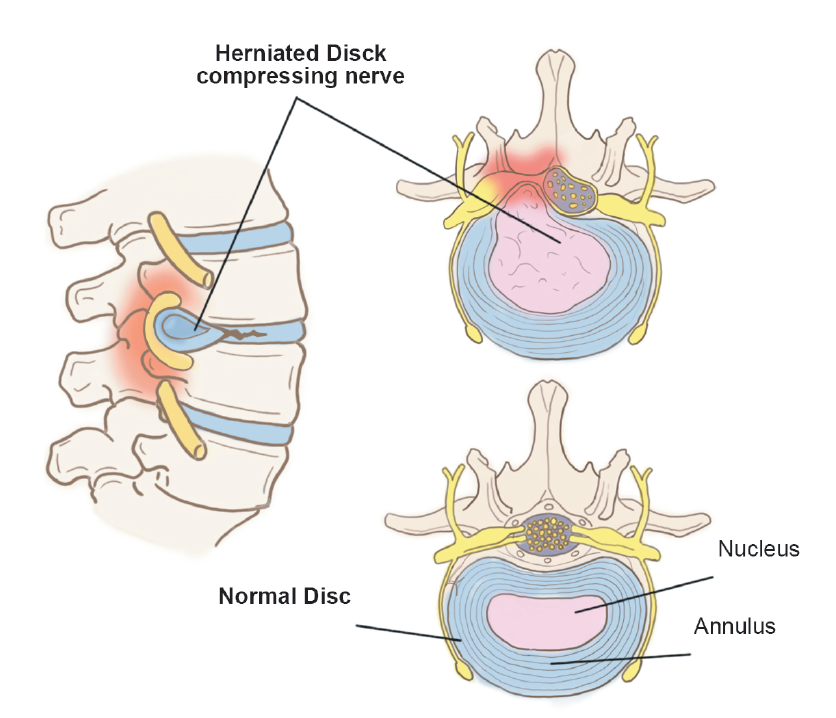
What is a Slipped Disc or Disc Prolapse?
When the intervertebral disc is compressed, it initially causes annular tears and ultimately cause the nucleus rupture, as the disc starts slipping due to the pressure exerted on the disc. This condition is known as a Slipped Disc or Disc Prolapse.
What is a slipped disc or disc prolapse?
What do you recommend once I am diagnosed with a Disc Prolapse?
It is tempting to rest and stop all physical activity due to severe pain from a disc herniation because of fear that the pain causes. However, this can lead to joint stiffness and weakness of the muscles. Remaining active by walking and stretching would provide much more relief. Initially, you may benefit from physiotherapy and adopting an exercise program to strengthen the core muscles while reducing pain. Pain killers and taking a break from heavy lifting and painful positions are also beneficial. I would usually recommend surgery if your symptoms last longer than six weeks and the pain is uncontrolled or if the condition is affecting muscle function.
When might I require emergency surgery?
The only absolute indication for surgery is for the cauda equina syndrome. This syndrome is a surgical emergency that often presents dramatically. The disc will press on the cauda equina, which consist of the nerve roots to the lower limbs, the bladder, and the rectum, causing the following motor and sensory problems:
- Loss of perianal sensation (around your anal opening) “saddle anaesthesia.”
- Bilateral weakness in the legs with often pain on both sides
- Sphincteric disturbance resulting in incontinence
- Inability to sense bladder filling, painless retention, and overflow: urinary incontinence Loss of anal tone: faecal incontinence
- Cauda equina is a surgical emergency requiring an emergency MRI scan and subsequent surgery and decompression. If the bladder and bowel is affected for more than 24 hours, surgery may be too late in reversing the symptoms; this is an emergency, and you should seek urgent medical advice or attend the emergency department without delay.
Other urgent indications for surgery are:
- Unrelenting leg pain despite adequate conservative measures
- Progressive neurological deficit
- Recurrent acute attacks of pain
What is a Slipped Disc or Disc Prolapse?
- There are risks of an anaesthetic and surgery, such as developing pneumonia etc. Elderly people have higher rates of complications from surgery. So do people with excess weight or medical illnesses such as Type 2 diabetes, heart disease, if you smoke or if you have multiple medical problems.
- You must inform my anaesthetist, the nurse looking after you, preassessment team and me of all the medications you are taking, any allergies that you may have including drug reactions as these can seriously impact your surgery and recovery. Drugs such as aspirin, clopidogrel, and other blood thinners may need to be reviewed or stopped under guidance before surgery. If you are diabetic, especially on insulin, this needs to be highlighted early.
- Do try if time permits to stop smoking, lose weight and make some lifestyle changes as these will make your recovery smoother.
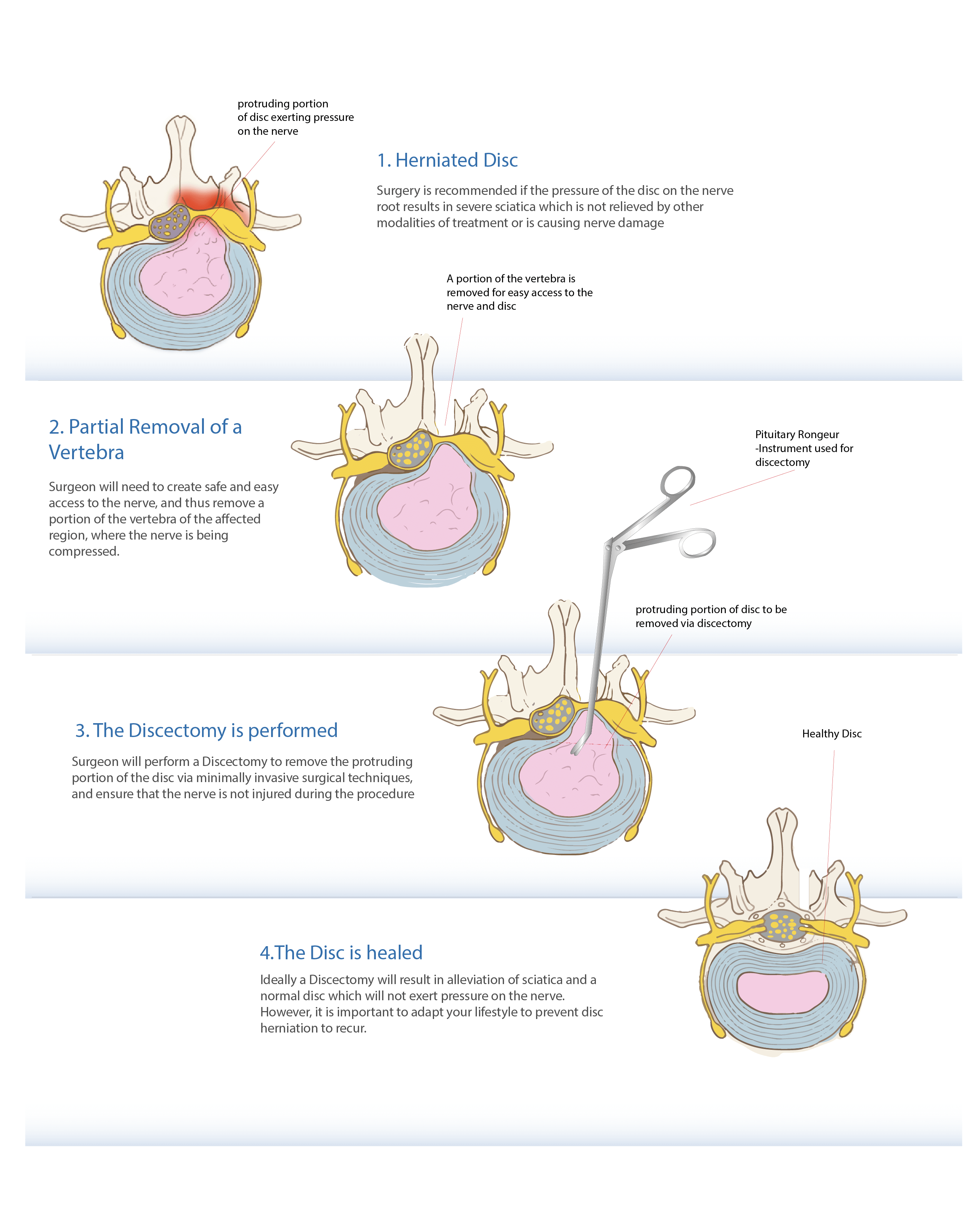
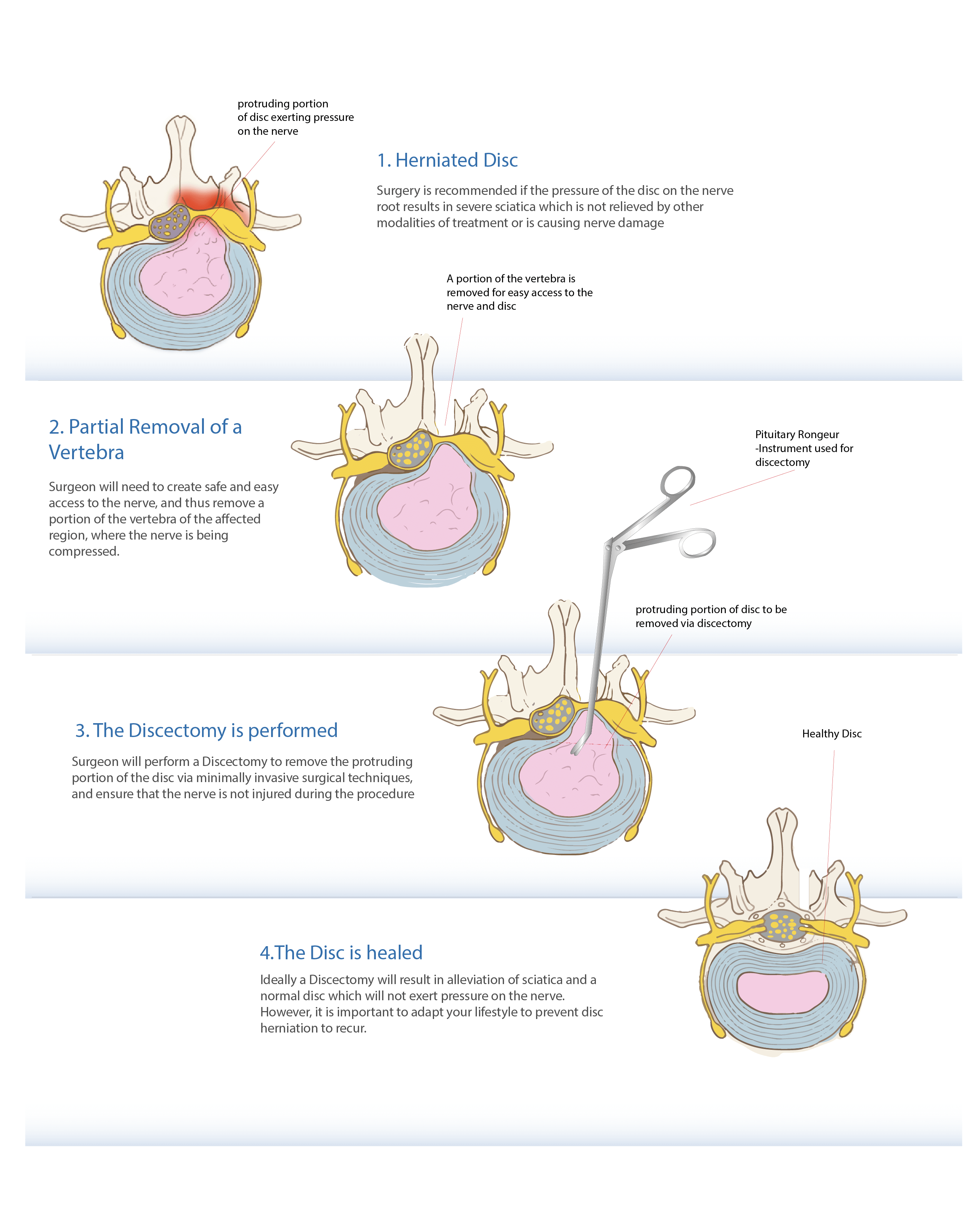
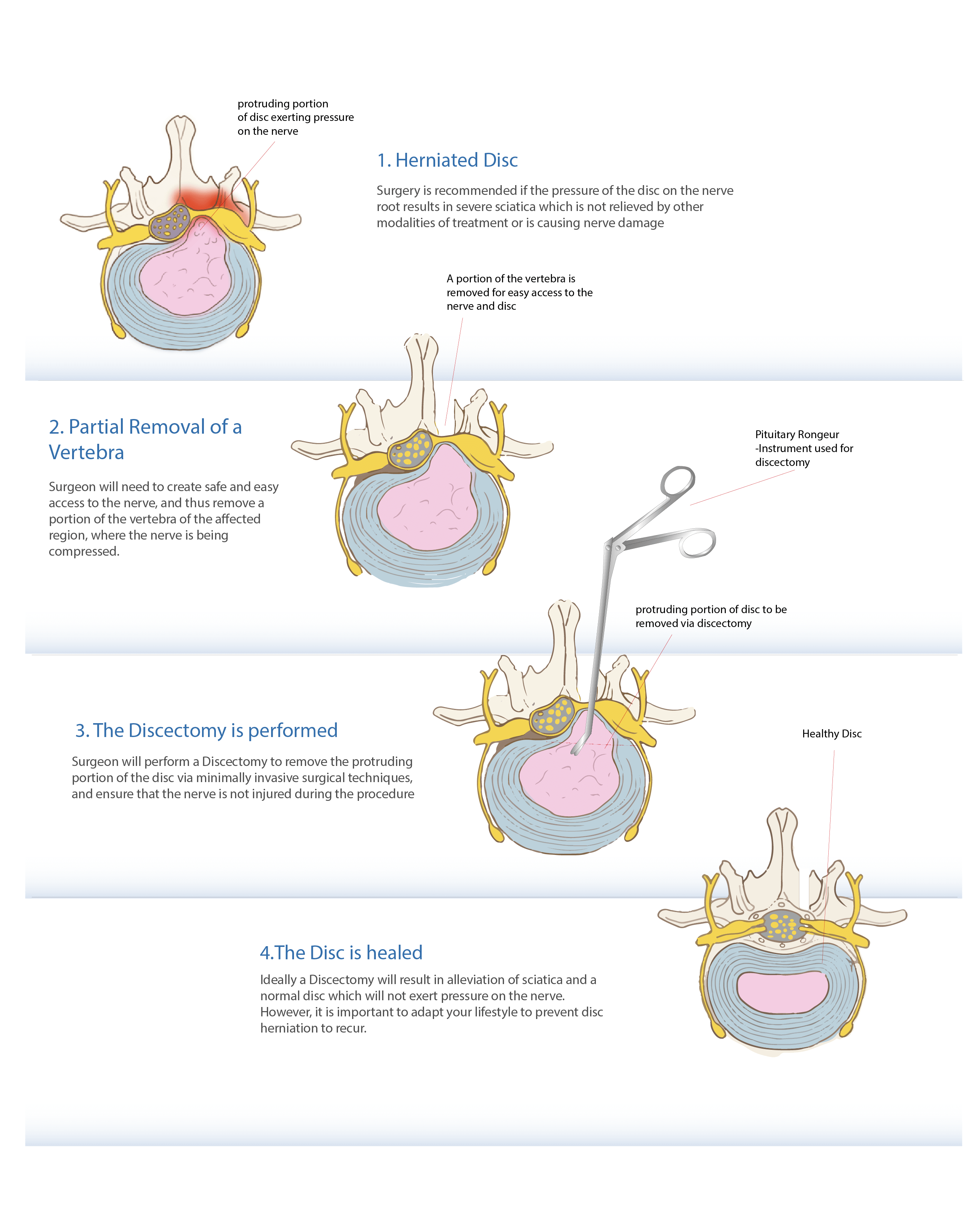
What is involved in a Discectomy?
Using high magnification with the help of a microscope or a loop, I perform the surgery under general anaesthesia. The procedure involves removing a part of the herniated disc to stop it from pressing on the nerve.
A 3-7 cm incision over the affected portion of the lower back is made to gain access to the involved nerve root and disc by removing a small part of the lamina and the surrounding soft tissue or ligamentum flavum. Then the protruding part of the disc compressing the nerve root is taken out, along with other loose fragments. Ideally, just the portion of the disc that is pinching the nerve is removed, relieving the pressure on the nerve but leaving most of the disc intact. The wound is then closed with dissolving sutures that do not need removal.
What are the risks of having a Discectomy?
Though the complication rate for a discectomy is uncommon at less than 1% (1 in a 100), here are some of the risks associated with the procedure which I will be discussing with you along with my own success rates:
- Infection: The risk of infection is less than 1%. All my patients receive a dose of intravenous antibiotics when they are going off to sleep. If you develop an infection, it is most likely to be a superficial wound infection that will resolve with a short course of oral antibiotics and not usually a cause for serious concern.
- Bleeding: Blood loss is usually minimal.
- DVT: Developing blood clots in the legs (deep vein thrombosis – DVT) is a risk of any surgery. The risk is minimised by using thrombo-embolic deterrent stockings (TEDS) and mechanical pumps. These pumps squeeze your lower legs, helping the blood to circulate. They are put on when you go to sleep and stay on until you start to mobilise. I encourage early mobilisation as this also helps to prevent DVT.
- Nerve Injury: This is an exceedingly rare but serious risk of a discectomy as the nerve is often already stretched and under tension due to the slipped disc and the nerve has to be taken to a side to remove the slipped disc. Nerves do not take handling and retraction very well and may be damaged to some extent and rarely a complete damage may result in weakness and numbness in the area supplied by the nerve permanently.
- Dural Tear: Rarely there can be an injury to the thin membrane that surrounds the nerves (Dural tear) which can result in a CSF leak. This can usually be repaired at the time but sometimes needs another operation to address it.
- Long term risks: There is a high likelihood that you will resume you normal lifestyle after your surgery and keep your pain under control. However, it is always possible for the disc to rupture again, which happens in 5-10 % (5-10 in 100) of patients up to 7 years after surgery.
How long should I expect to stay in hospital?
The procedure involves an overnight stay in the hospital, usually for a day.
What should I expect after a discectomy?
Local anaesthetics used around the wound at the time of surgery are usually adequate for managing pain. Occasionally intravenous pain killers are used together with tablets to keep you comfortable. A physiotherapist will visit you to teach some basic exercises. You will be asked to walk up and down stairs to ensure normal mobility before you are discharged from the hospital.
I recommend that you avoid driving, excessive sitting, lifting, or bending down for about a month after surgery. Be guided regarding how much you move or bend in the first few weeks after surgery based on your pain. If it is painful, be careful of overdoing it. Your physiotherapist and I often demonstrate exercises to strengthen the back and to prevent scar formation around the nerve (nerve flossing).
Following a hospital stay, you are given a physiotherapy program before discharge to help recover.
What should I expect at home?
- The treating physiotherapist usually provides exercises that you can follow easily at home. The ward team will prescribe pain-relief medicines. Non-steroidal anti-inflammatory drugs (NSAIDs) are not always prescribed as they can cause oozing from the wound.
- Stool-softeners. These are sometimes required initially to in to avoid constipation which would prevent excessive straining during bowel movement.
- Look after your wound by avoiding activities like bathing, swimming, and hot-tubs until the incision has completely healed to prevent rupturing of sutures and infection from setting in. The absorbable sutures used for surgery usually dissolve in a few days after surgery. A water proof dressing is used to cover the wound to allow showering. Do ring the ward if you have any concerns.
- You should continue with the physiotherapy program and follow the prescribed exercises. You should avoid activities like running or lifting heavy weights (typically over 5 pounds).
- You are advised to use compression stockings to prevent blood clot formation, until you are completely mobile.
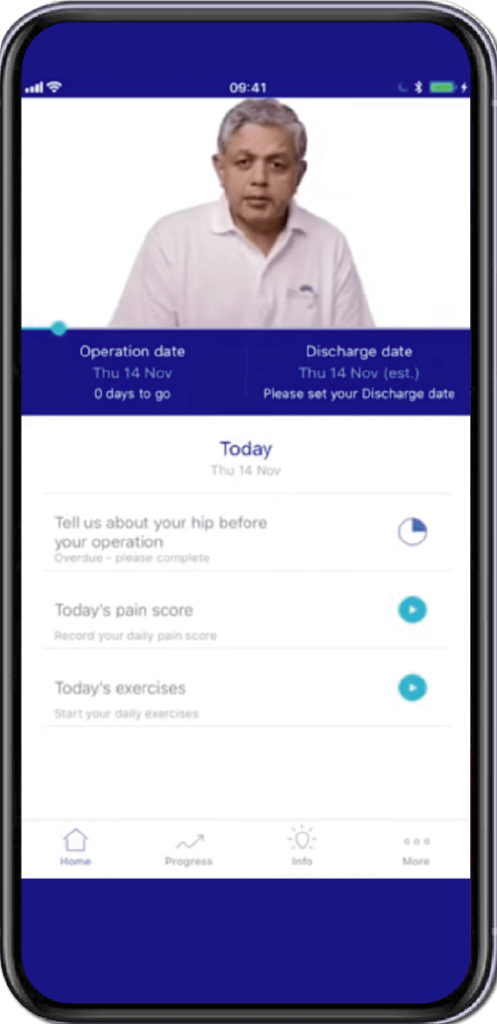
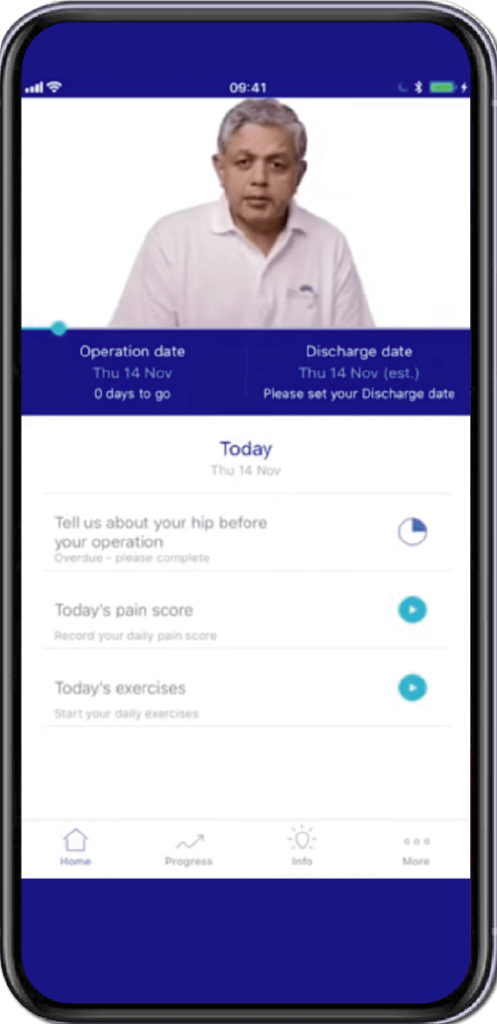
- I would like you to download and use the link to the app for MyRecovery to collect information which helps me improve my service (https://www.myrecovery.app/rba)
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
