
Low BACK PAIN
Most people experience pain in their back at some point in their lives. Usually rest and pain relief medications ease the pain. When the pain is persistent and present at rest, it can be an indicator of a more serious underlying condition.
What is Low Back Pain?
Is there an evolutionary cause?
Our spine has normal curvatures that balance each other and allow us to walk upright with the centre of gravity falling between our feet. For most of the period human beings have been on the planet and until the Industrial revolution (1760-1840), we were much more physically active. This changed our lifestyles and in more recent times we are more sedentary than ever before. Our food habits have changed from mostly fruit and vegetables to the current western diet typically consisting of over 50% of ultraprocessed foods full of fat, sugar and salt. Our intake of animal derived foods has increased dramatically and in general, we are a much heavier nation.
Since World War II, back pain is considered a disease and often managed as one, rather than just a symptom. In modern medicine, we always like to find ‘a cause.’ There are in fact, many factors that are responsible for back pain.
How do we identify a cause for our back pain?
Discogenic Back Pain
This is the most common cause of lower back pain. The syndrome originates commonly from a lumbar disc (pain generator)
Broadly, degenerative disc disease (DDD) is often the cause of back pain
How is back pain treated?
It is often by taking a detailed medical history and clinical examination of the patient that we, as doctors get a good idea about what is the cause of low back pain. You may be also advised to have an investigation such as an MRI of your spine or hip, X rays, blood tests depending on what would be the most helpful in your treatment. You can help by having details of your symptoms as well as any previous medical history, medical records and treatments including details of medications to hand.
Broadly speaking, back pain is usually categorised as either a serious cause or a mechanical cause. The intensity of pain is not always a reason to worry that the cause is sinister. In fact, most back pain is not serious or sinister in nature. Mechanical causes often have a background of reduced activity and prolonged sitting in a poor posture, in other words being sedentary.
As in many lifestyle related causes, addressing the root cause helps with the back pain. It may not be a pill or an intervention that will help in the long term. Movement and exercise help especially as the nutrition of the disc, being avascular (no blood supply), depends on its nutrition from the surrounding bone.
What are ‘Red Flags’ in Back Pain?
I like to think of these as red flag symptoms (which you as the patient may experience) and red flag signs which your doctor elicits. Red Flags may point to a serious underlying cause of back pain. The important serious underlying causes are neurological emergencies such as ‘the cauda equina syndrome’, paralysis or weakness, spinal infections, cancer (usually ‘secondary cancer deposits’ with the origin of cancer elsewhere, such as breast or prostate) or pathological fractures caused by Osteoporosis (hyperlink).
Red Flag Symptoms
If your pain is severe at rest, particularly keeps you awake at night or wakes you up from a deep sleep, needs urgent medical advice and investigations to rule out underlying causes. Pain that is not responsive to common pain killers and requiring stronger pain killers is also a cause for concern. Also, back pain symptoms that worsen with time and with rest should not be ignored.
Mechanical back pain, on the other hand, is notable in that symptoms usually get better with the passage of time. Neurological symptoms such as weakness of limbs or definite numbness especially around the anal opening (back passage) or loss of ability to feel the bladder filling up with urinary or faecal incontinence are extremely worrying symptoms. Systemic symptoms such as unintended loss of weight of 10% or more of total body weight, loss of appetite, fever and night sweats often indicate an underlying serious condition and need urgent medical input and often specialist referral.
Sudden onset severe pain after a particular action such as lifting a heavy weight or doing unaccustomed exercise is often a first presenting symptom of an annular tear discussed below, and a short period of rest (24-48 hours) is often enough to generally calm it down.
Red Flag Signs
Neurological issues are easily identified as these usually result in objective numbness or weakness that can be demonstrated. Some of the other conditions are more subtle as the spine lies quite deep and inaccessible to physical examination. Symptoms and taking a good medical history are often the key.
In osteoporotic fractures, percussion or tapping with a closed fist can cause micromovements and therefore pain. Patients with infection are often in very severe pain and can be difficult to examine. Any concern about the serious nature of your back pain will usually need further urgent investigations such as an MRI scan, CT scan, blood tests or X rays.
I experienced severe pain and my ‘back went’!
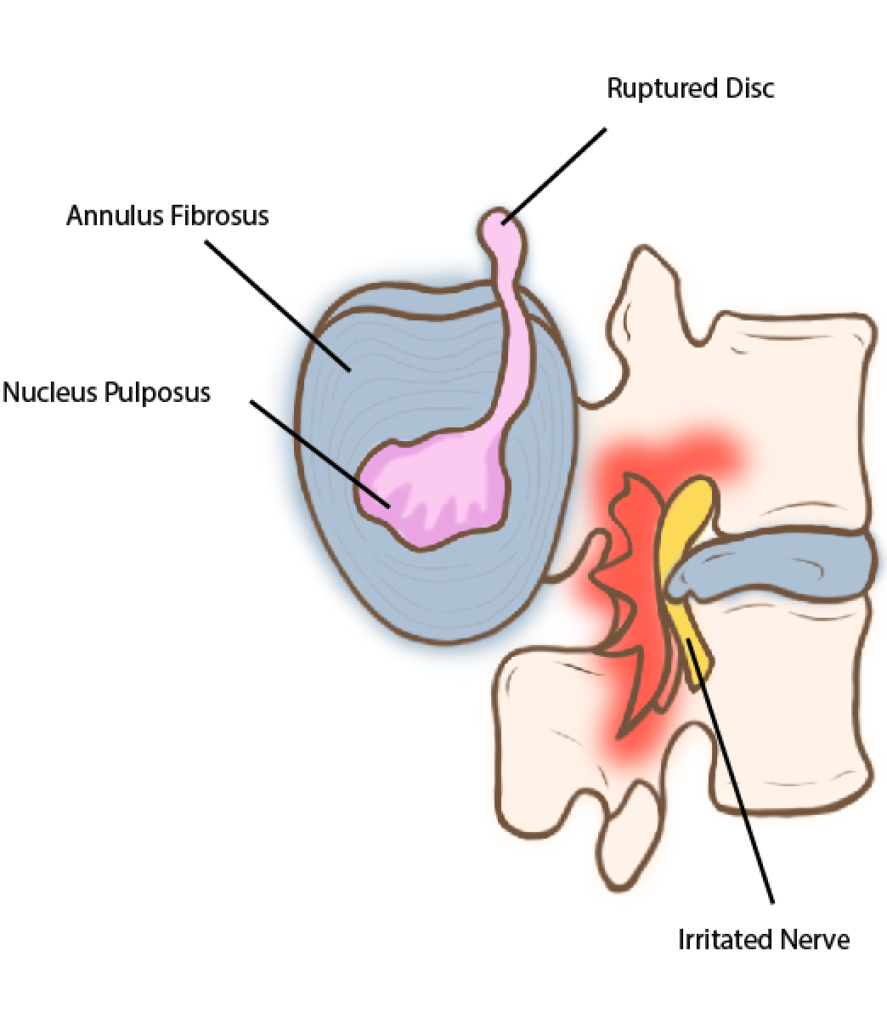
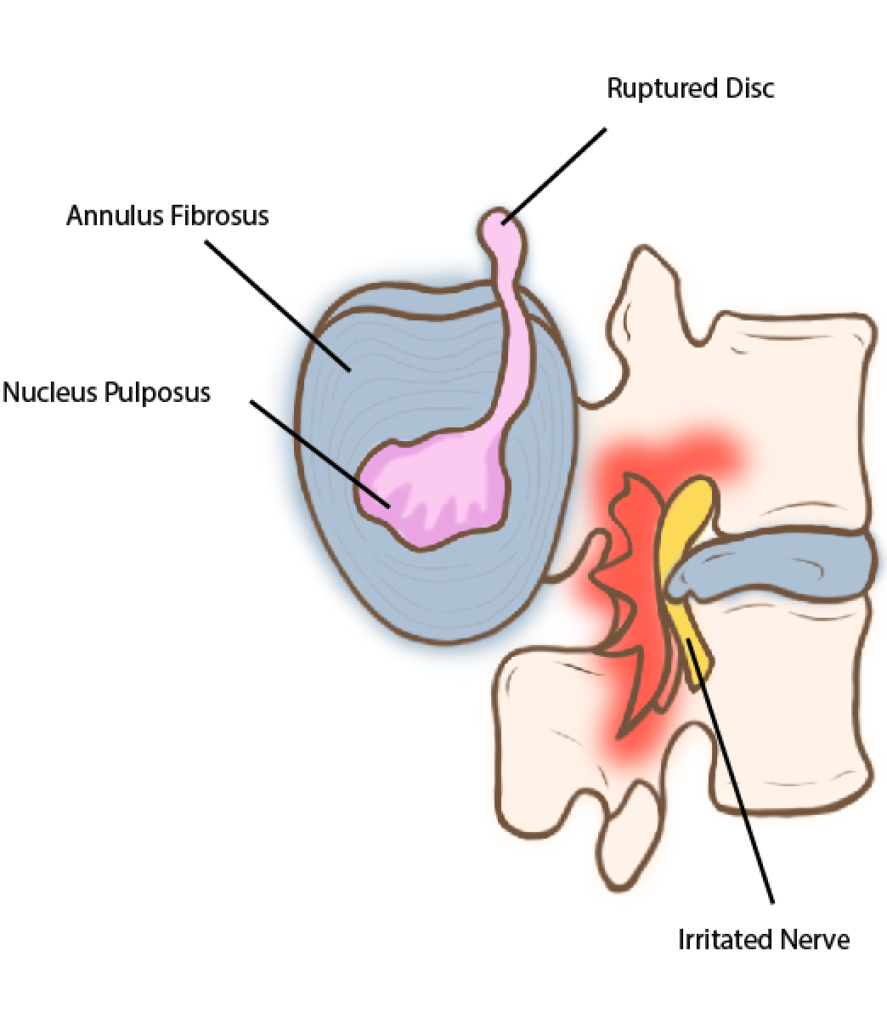
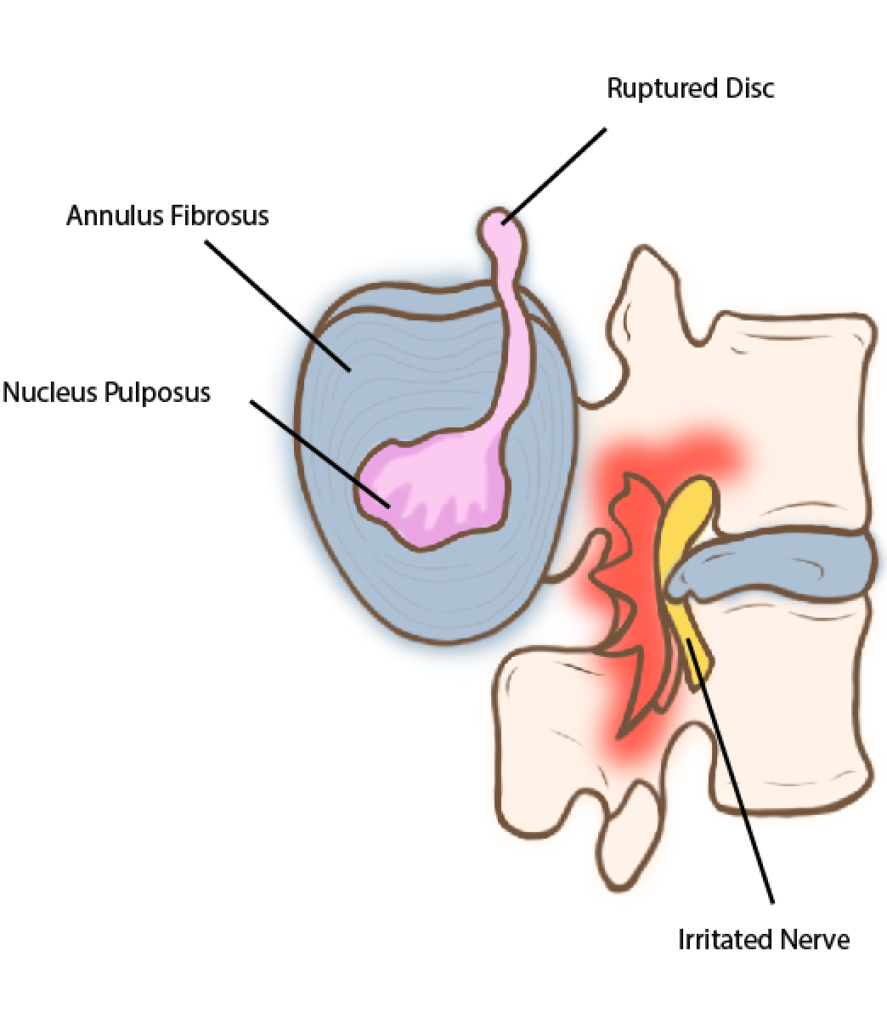
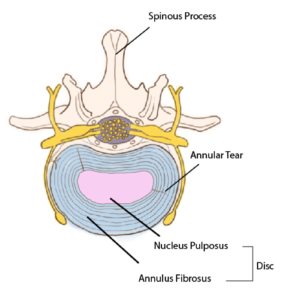
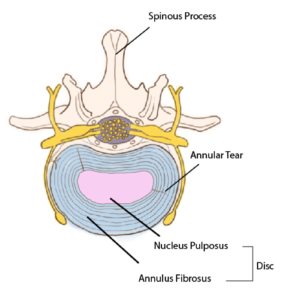
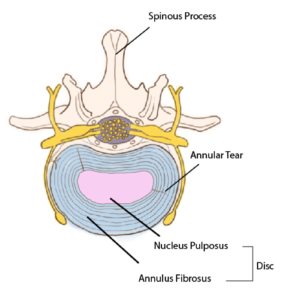
While the pain can be very intense and crippling, this common mode of presentation which can be terrifying for you, is often due to a benign cause such as an ‘annular tear.’ This is akin to having a drop of boiling hot water scalding your hand. Exceedingly painful, but not dangerous, and usually heals with time. It is because the annulus of the disc has a rich nerve supply, and the ‘blister’ or tear allows inflammatory substances called cytokines to worsen the pain and inflammation at the site, as it heals. This can also lead to some neural irritation and symptoms referred to the groin and numbness in the legs or around the back passage and rarely may present mimicking ‘cauda equina syndrome’(hyperlink). Examination and certain tests can differentiate the two.
This can take a few days to months and is often better to prevent as treatment is harder once pain pathways are established. Occasionally an epidural type of injection to break the pain cycle or the help of a physiotherapist, Osteopath or Chiropractor can be especially useful in providing pain relief.
What should I expect after an acute severe episode of pain?
This can take a few days to months and is often better to prevent as treatment is harder once pain pathways are established. Occasionally an epidural type of injection to break the pain cycle or the help of a physiotherapist, Osteopath or Chiropractor can be especially useful in providing pain relief.
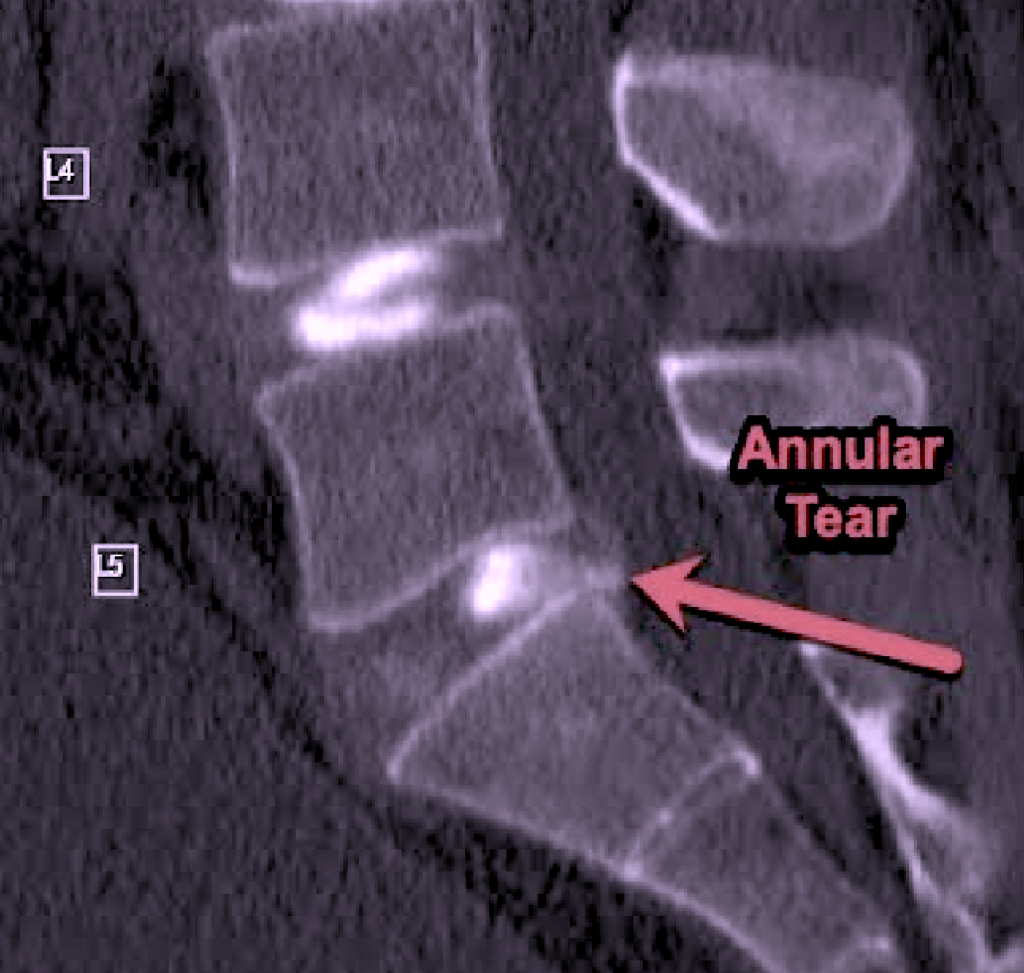
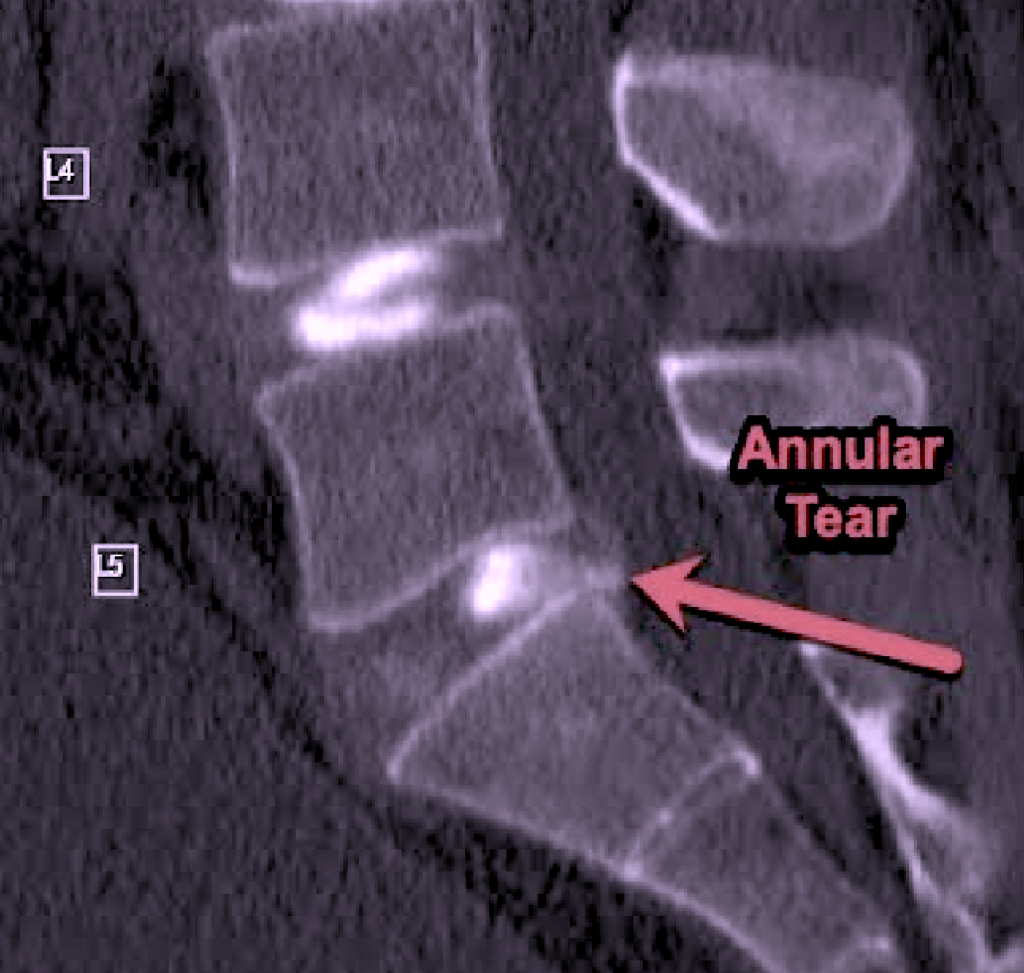
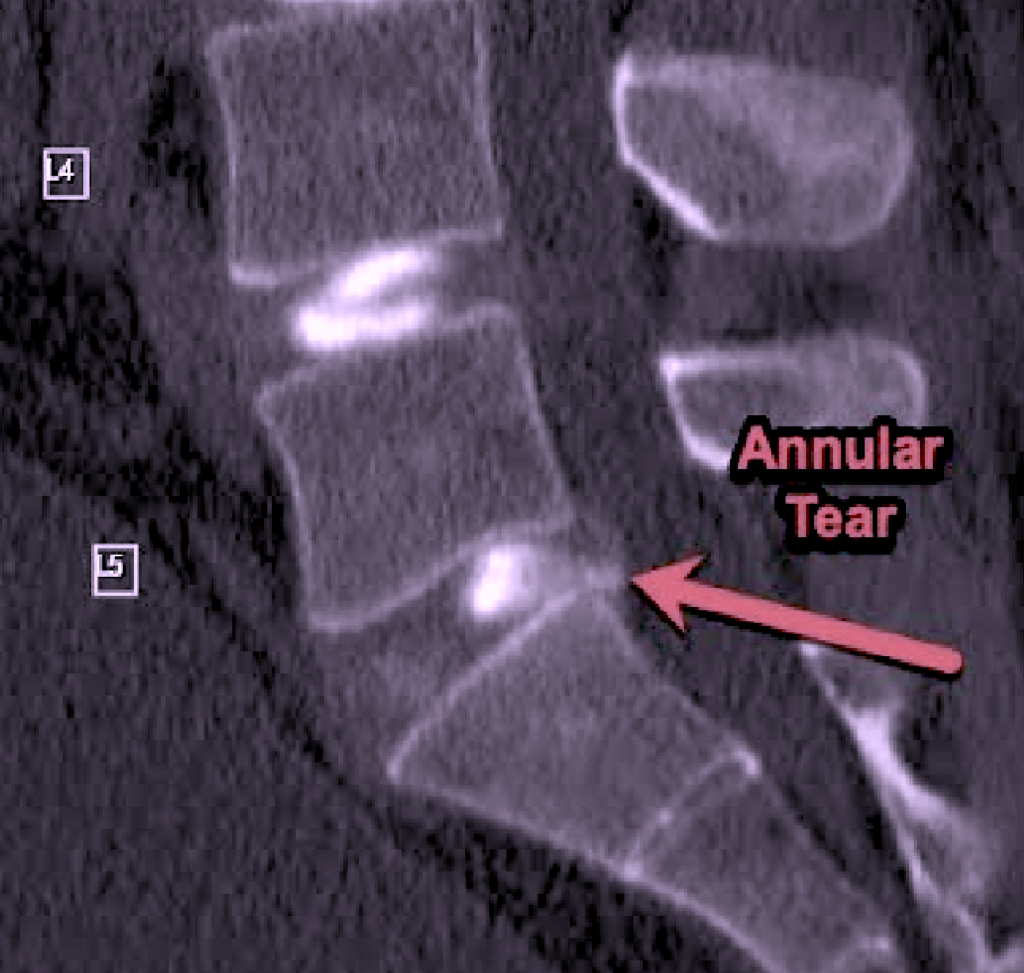
Annular Tear
When the Annulus Fibrosus is ruptured, it can cause extremely intense and crippling pain
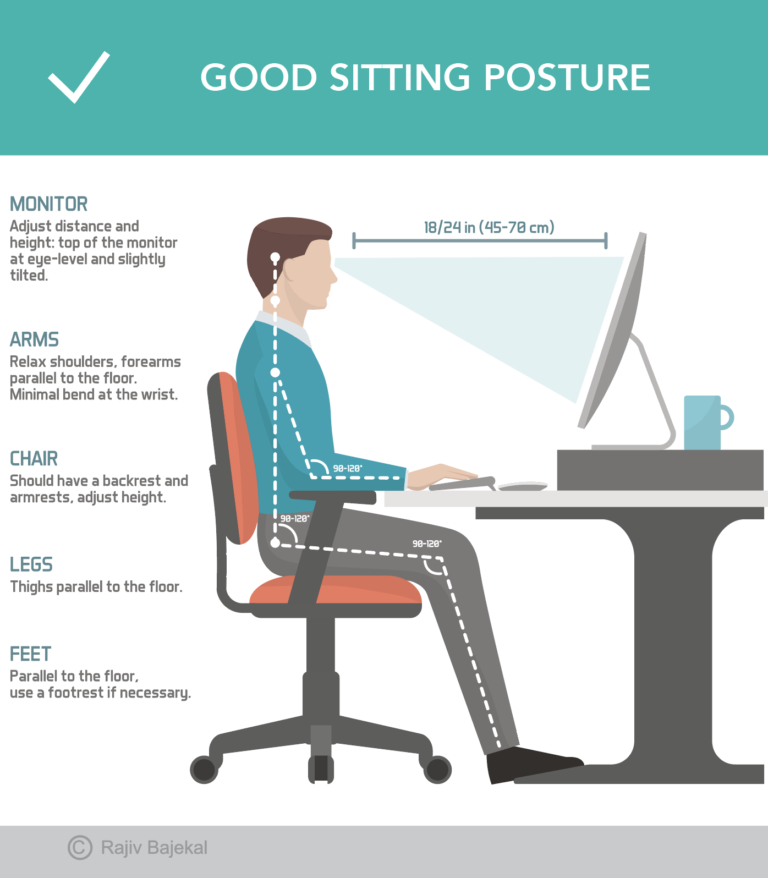
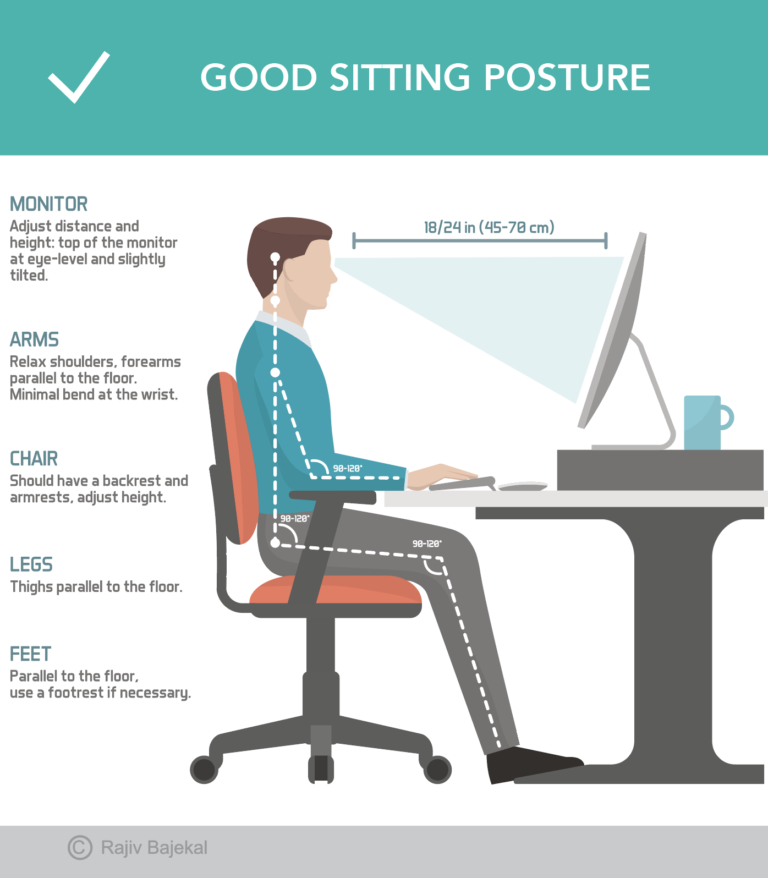
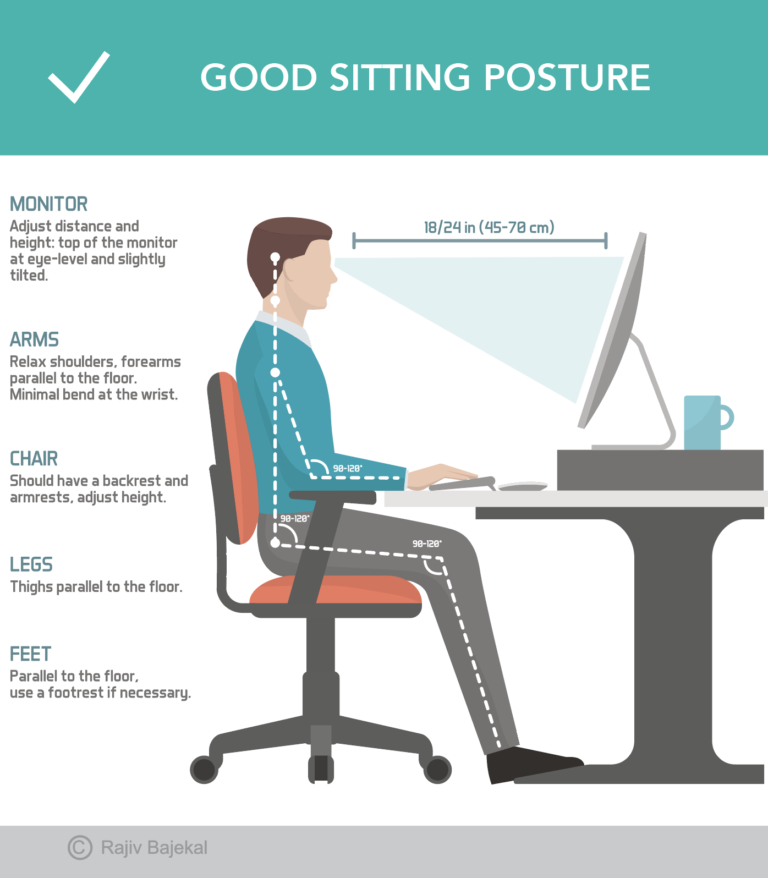
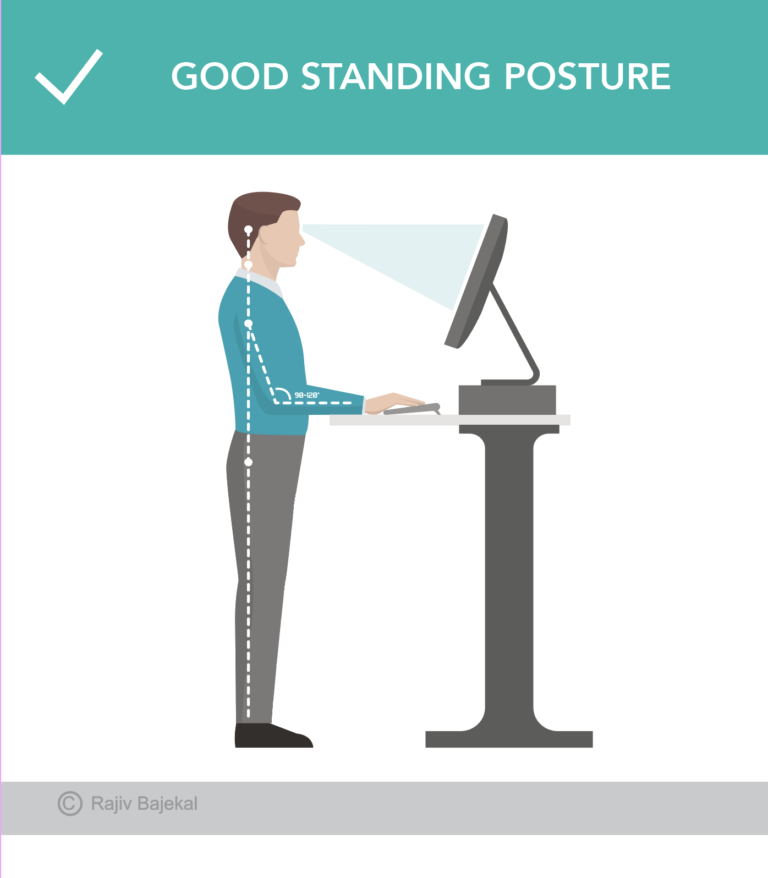
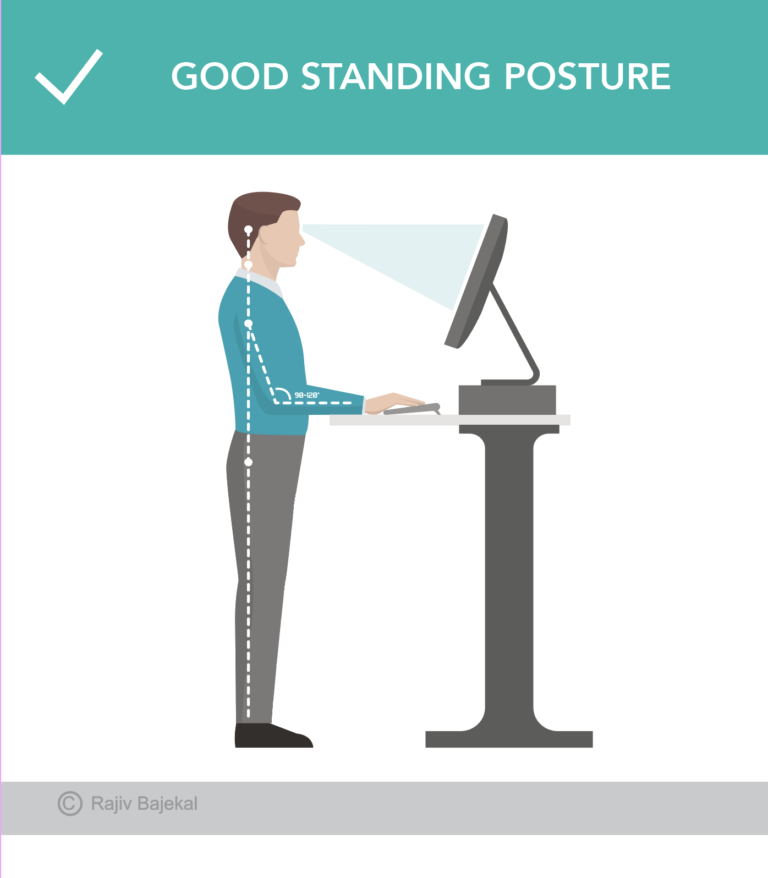
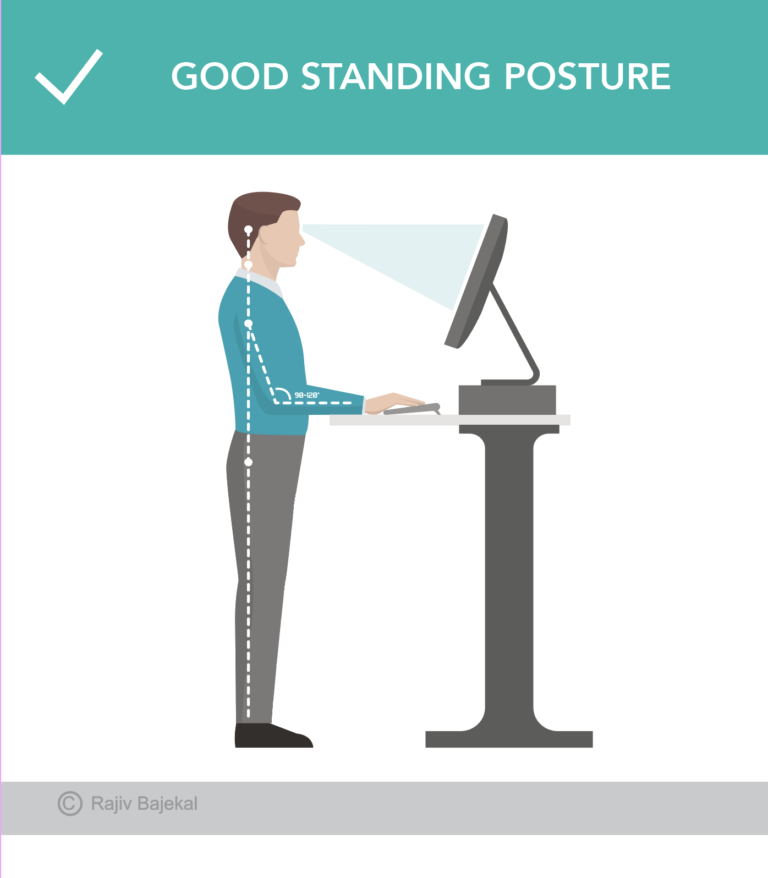
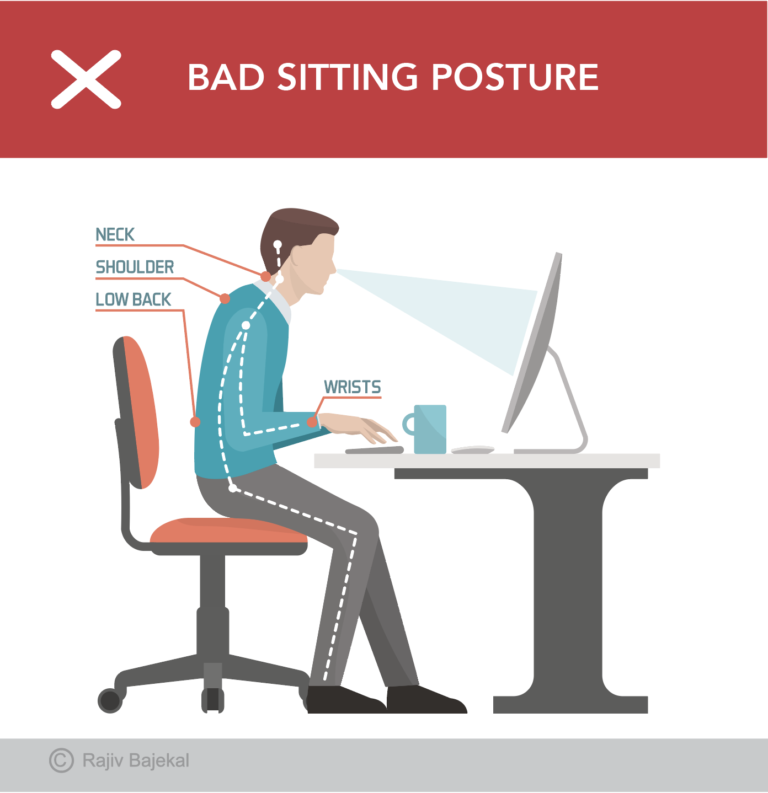
Is there a relationship between Posture and Back and Neck Pain?
Our sedentary lifestyles have meant that the spine is subjected to asymmetrical loads usually because of bad postures adopted over time. Slouching or sitting at a computer station all day where attention to posture and ergonomics has not been optimum is the commonest cause of neck and back pain. It is exceedingly common to flex the neck while texting and protraction (sticking out) of the neck, especially when fatigue sets in and one is working on a computer. This can add a 4.5-5 kg weight on your neck (cervical spine) that overloads the front of it, causing asymmetric wear and tear over time, leading to inflammation and pain.
The best way to understand a good posture while working is to stand against the wall so that your heels are against it while your bottom and the back of your head touch the wall. This is not the way we work as most of us are sitting down all day. At the very least we should be conscious that our heads are not poking forward, and our back is well supported against the chair. Standing desks are a step in the right direction but even taking a stretch and walking after every 20-30 minutes of working at a desk are an improvement. Workstations should be as ergonomic as possible.
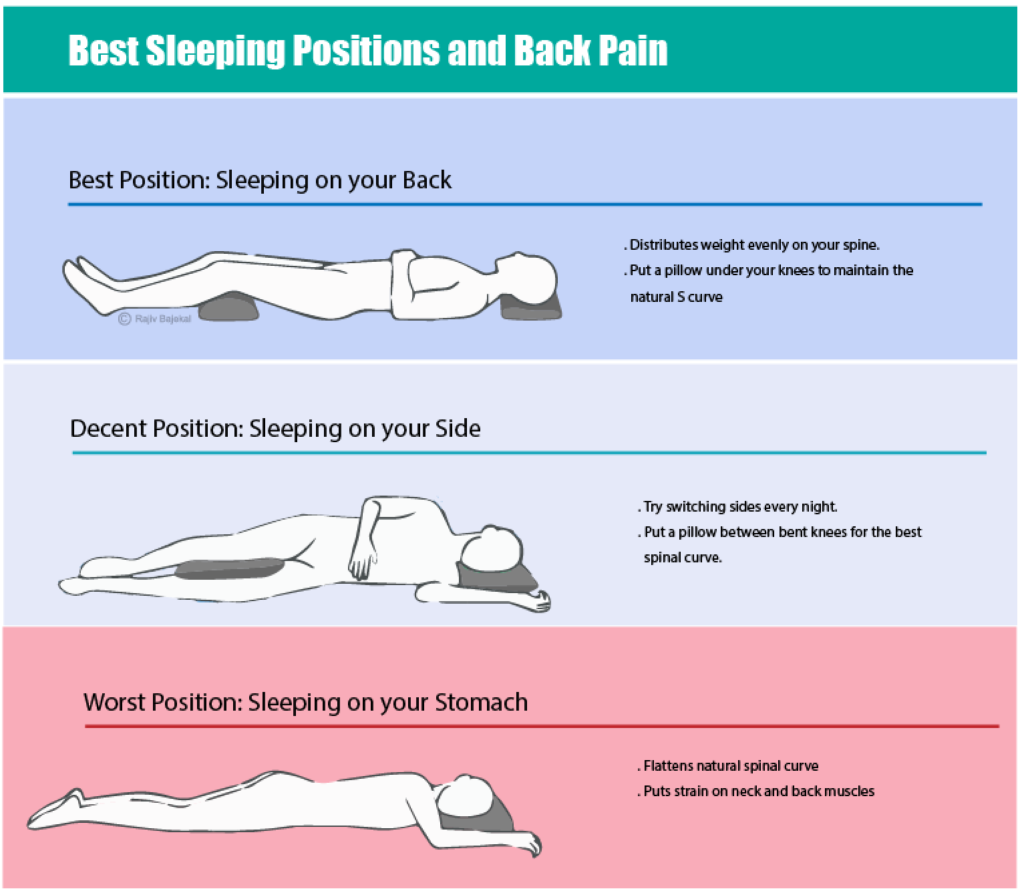
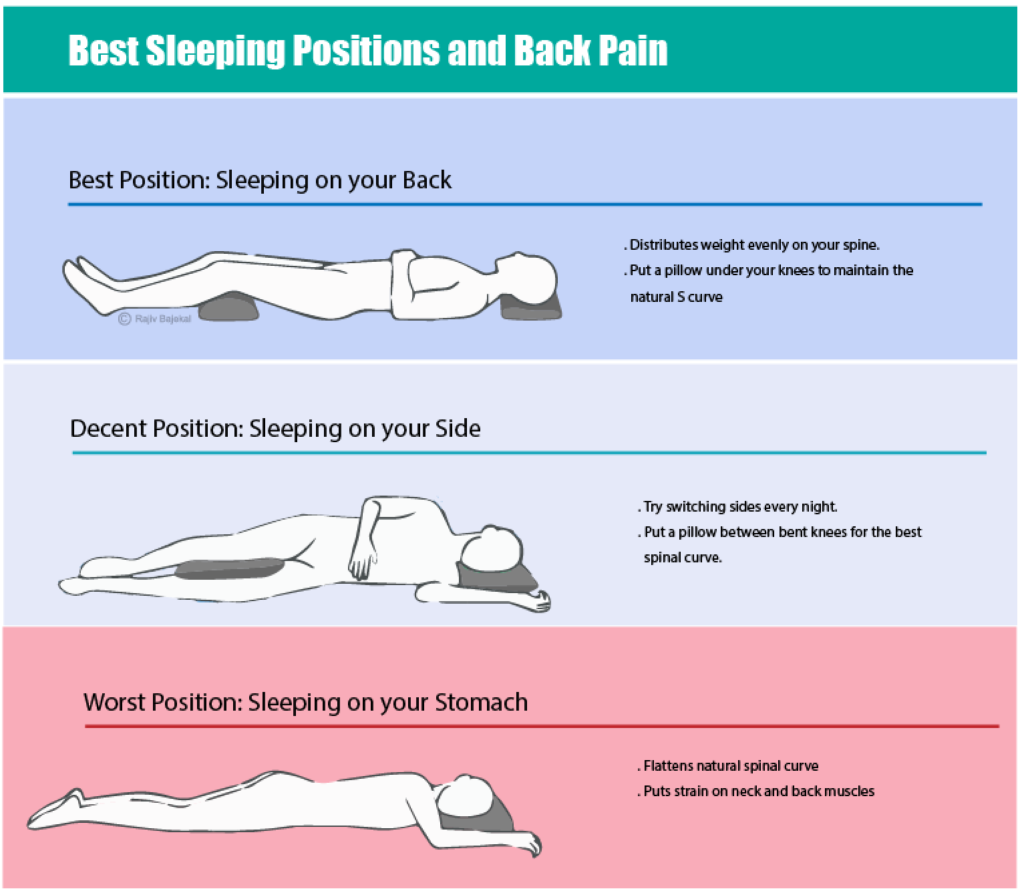
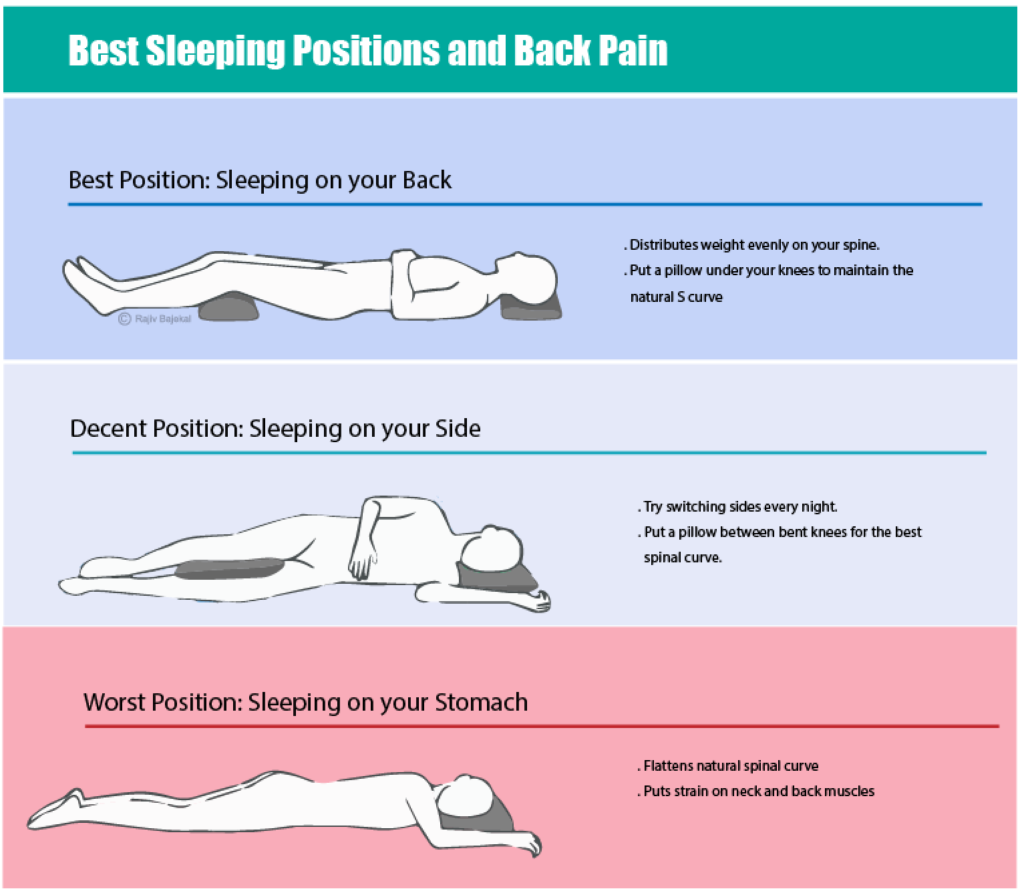
What posture should I sleep in?
We spend a third of our life sleeping and it is important to get a good restorative sleep for the body to repair itself. If the back hurts for longer than 5 minutes on waking up, one needs to think about the way one is sleeping. It is important to get a suitable mattress and pillow and these are a good investment. A mattress should not be too hard or too soft and a single supportive pillow is probably best. When lying down on the back, one should be able to pass the palm of the hand under the lumbar spine although not too easily. One should not feel any pressure on the bony prominences. If lying on the side, it is best if the hip areas do not feel the bottom of the bed (too soft) and there should not be any pressure on the shoulders or the hips- too firm.
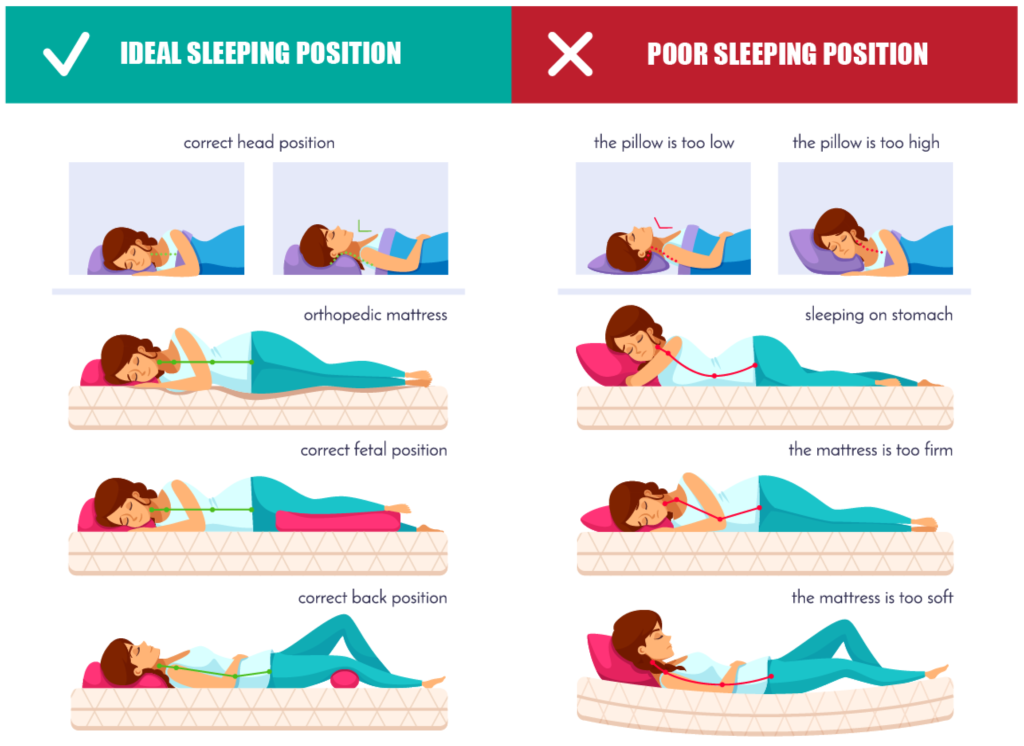
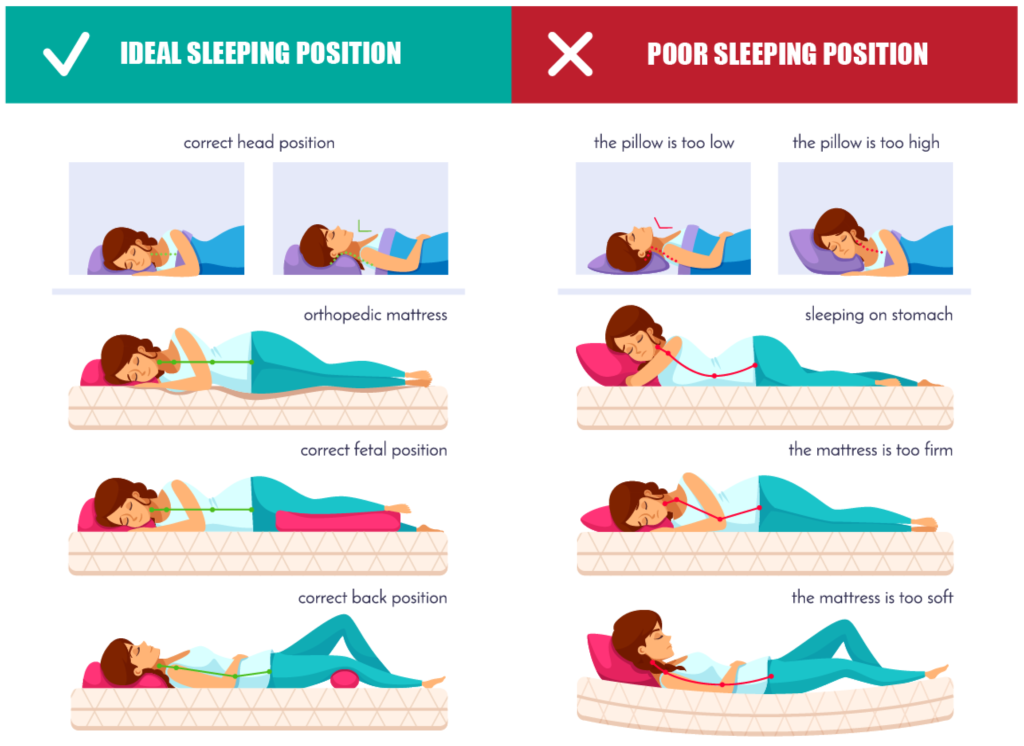
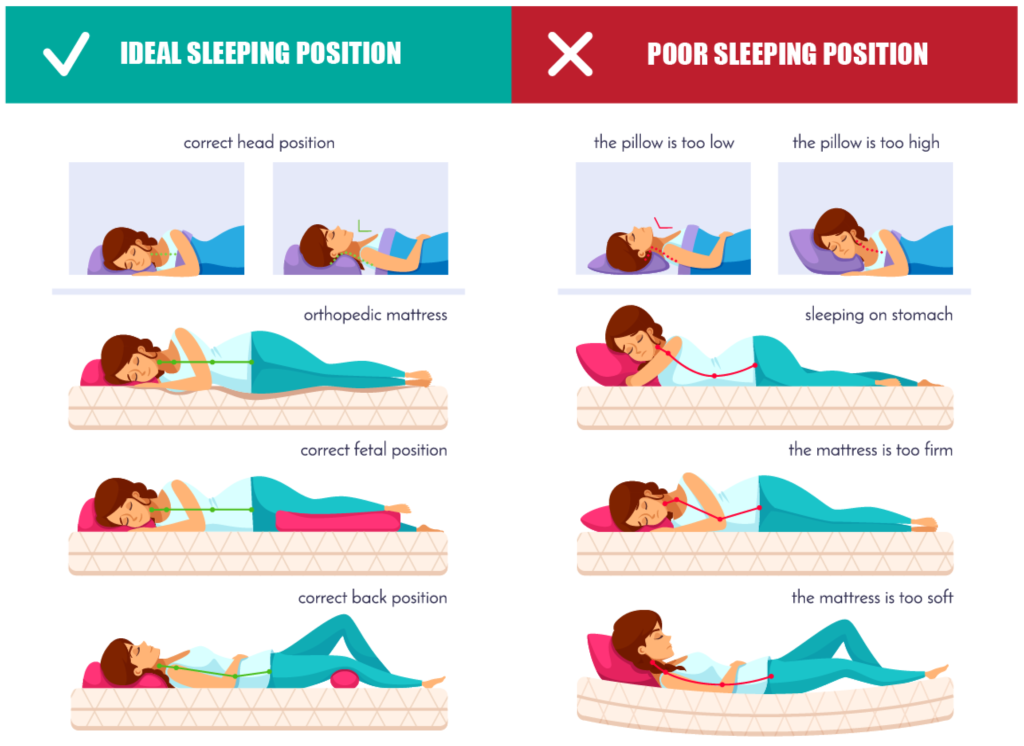
A pillow should allow your chin to be in the neutral position when you lie on the back and if lying on your side, it should bring the top of the shoulder in line with the head. A memory foam mattress and pillow generally work well for most people.
During sleep, there is inevitably a change in posture, but it is important to get a good comfortable starting position. People sometimes believe sleeping on the hard floor is the only way they get relief of their back pain. While this may give some temporary relief, there is certainly no benefit in subjecting a curved spine to a rigid surface, it will only put more pressure on the pressure points!
Are there any simple exercises I can do to improve my back and neck pain?
To understand why certain exercises work in helping prevent back pain and alleviating pain, it is necessary to understand what the common causes of back pain are. From an evolutionary point of view, we spent a lot more time moving previously, so regular physical movement throughout the day and regular stretches will help us keep the best posture to maintain the normal curves in the back.
During our generally sedentary jobs, we spend a lot more time in flexion and as we fatigue, often sitting in non-ergonomically assessed chairs, we tend to spend much more time with our spine flexed rather than in extension. From the time when we get up to the time we go to bed, we flex our spines into a C shape 3500 times per day! That is why it is ideal to have a stretch and walk around after every 20-30 minutes of sitting, however good one’s chair is!
What are the best exercises to prevent back problems?
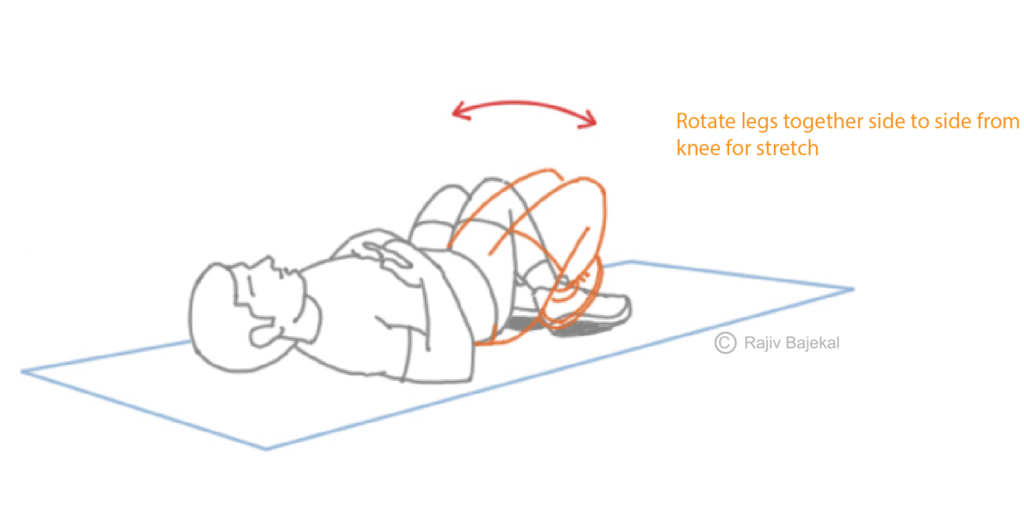
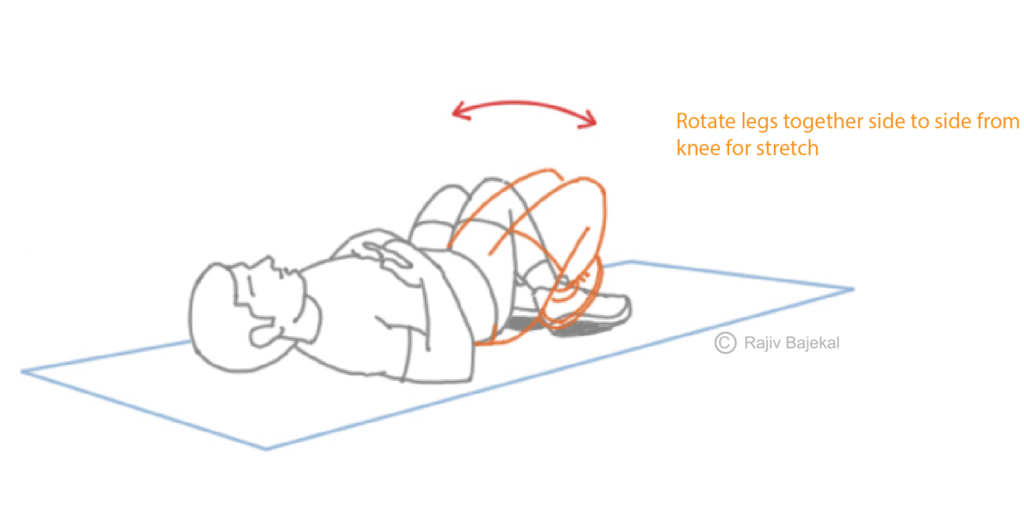
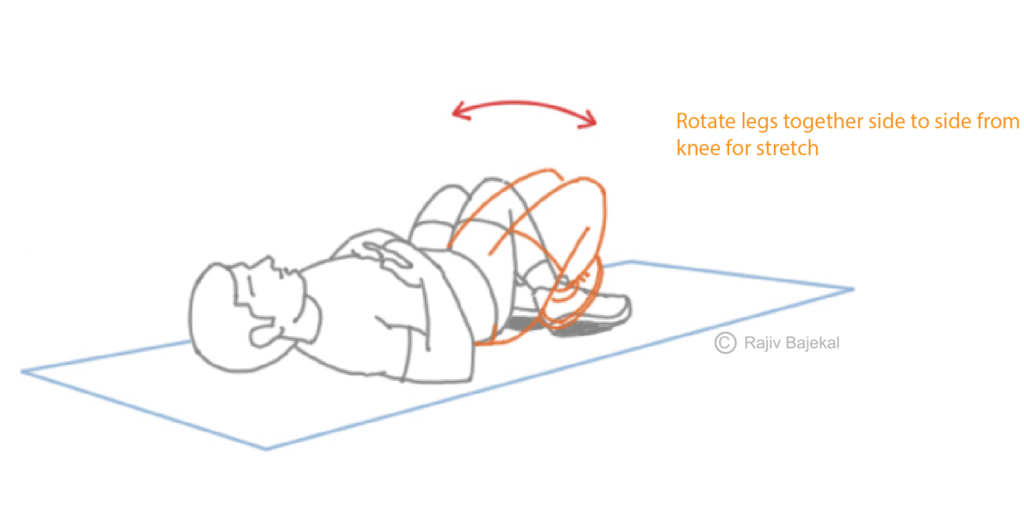
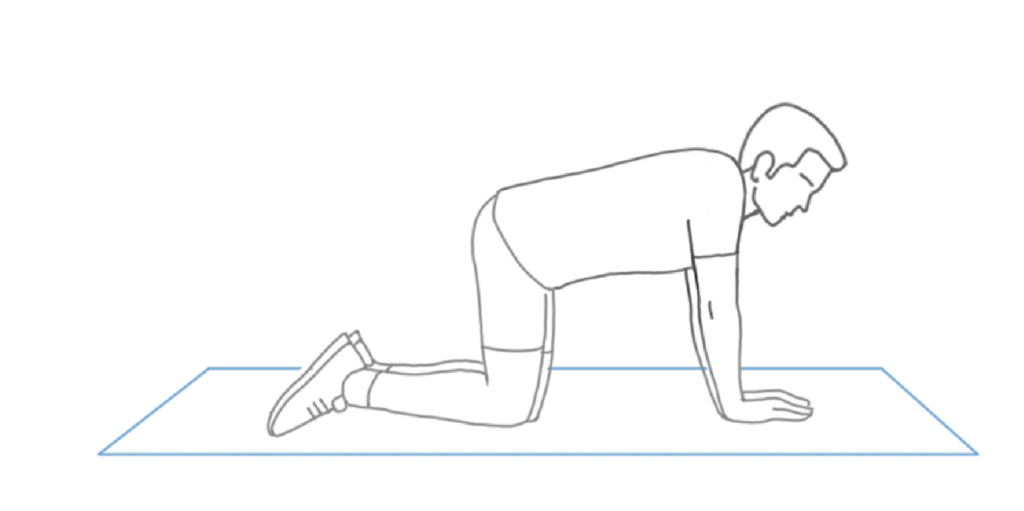
2. Childs pose (yoga pose) and stretch-Begin on all fours. Sit your hips back while reaching out your arms forward until a mild stretch is felt in the back. Hold the stretch for 10 seconds, repeat 5 times.



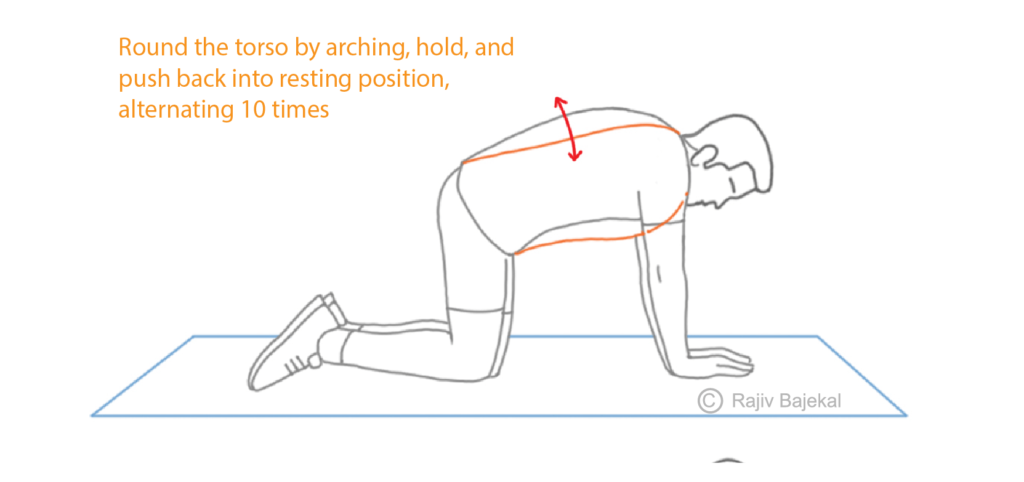
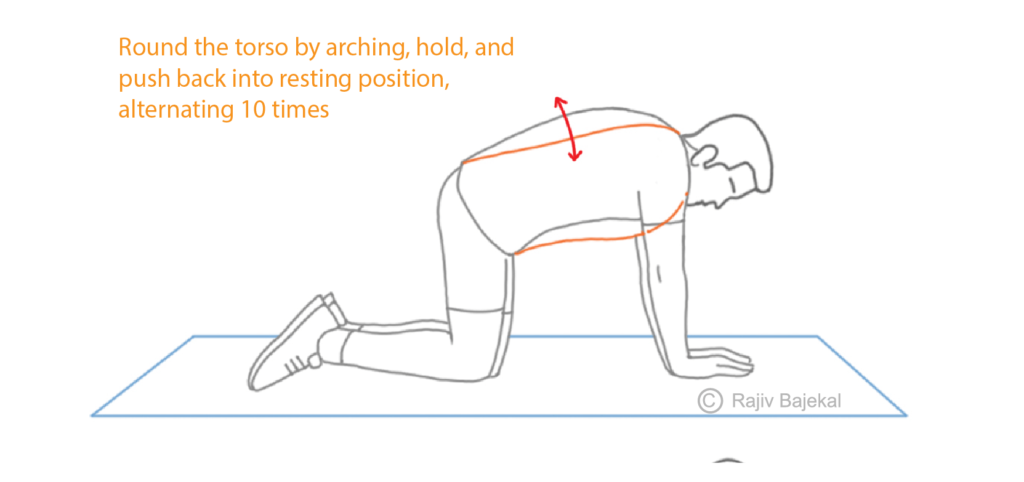
3. Cat-Cow stretch- Begin on all fours. Arch your back towards the ceiling and hold. Then arch your back towards the ground and hold. Hold each stretch for 5 seconds, repeat 10 times.
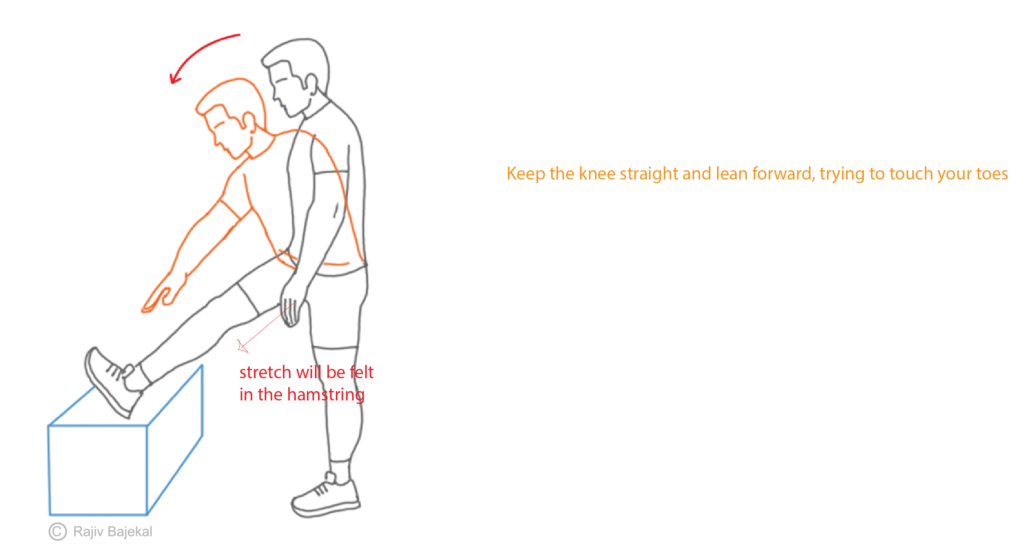
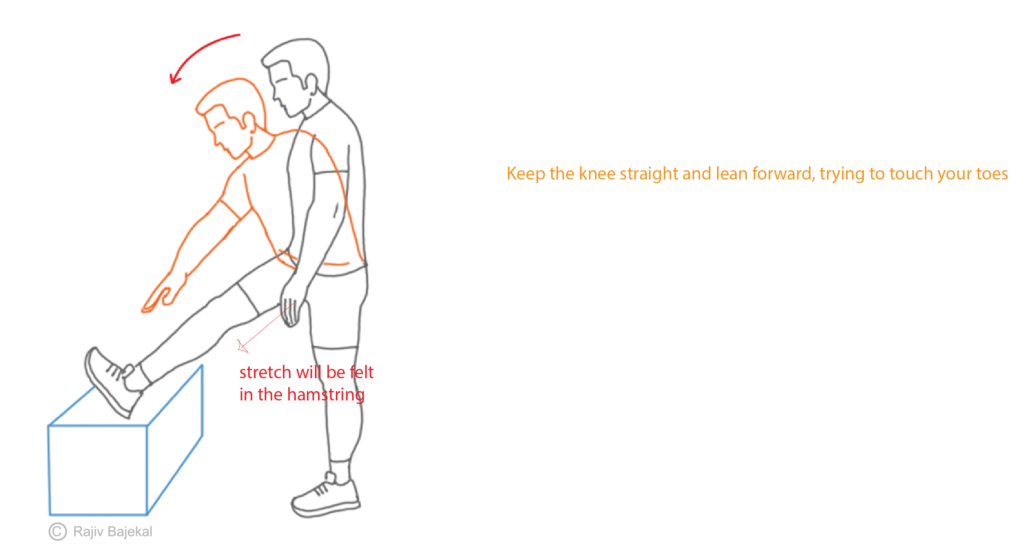
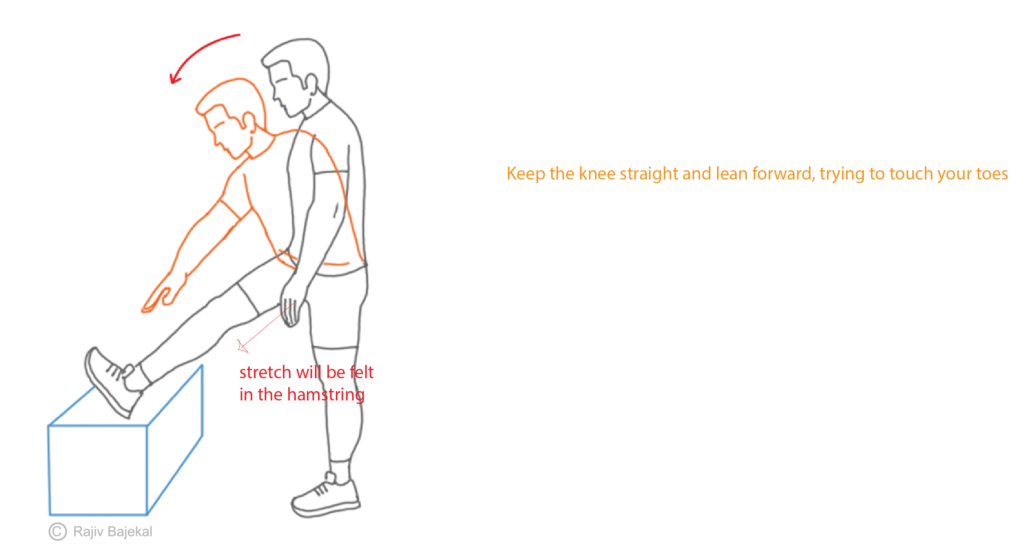
4. Hamstring stretch-Begin sitting on the floor with one leg straight, and the other bent. While maintaining a flat back, lean forward by hinging from the hip until a stretch is felt behind the thigh. Repeat on the other leg. Hold each stretch for 10 seconds, repeat 5 times.
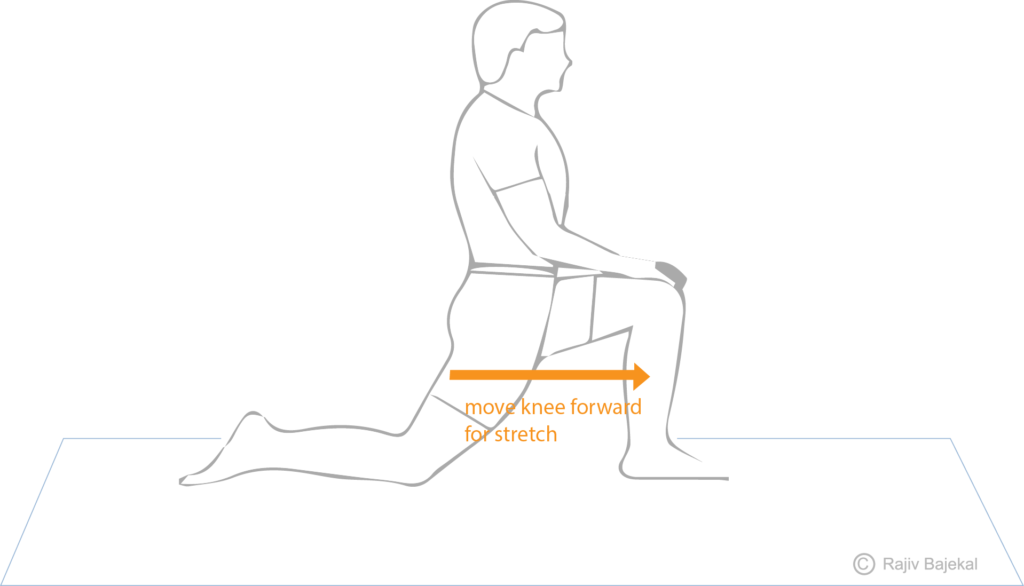
5. Hip flexor stretches-Begin by kneeling on a mat. Lean forward towards the bent front knee until a stretch in front of the opposite thigh is felt. Hold the stretch for 10 seconds, repeat 5 times.
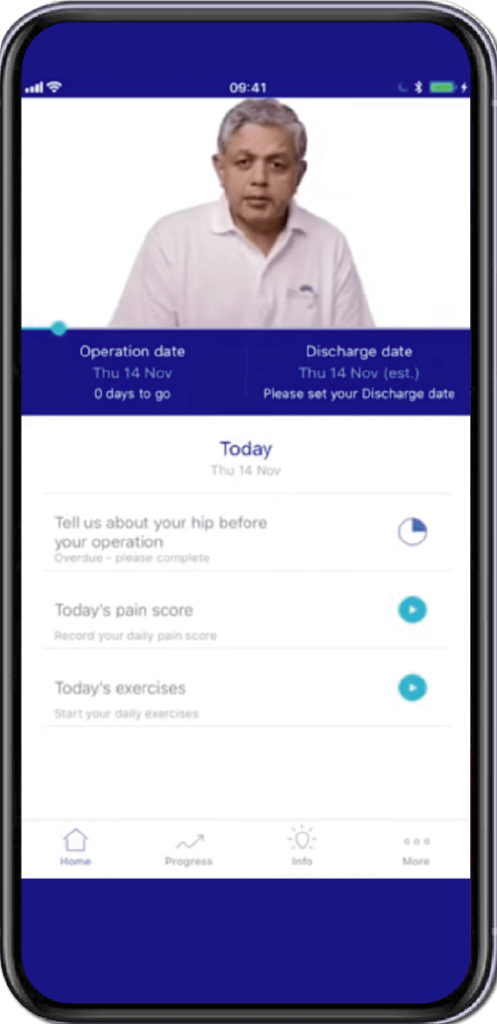
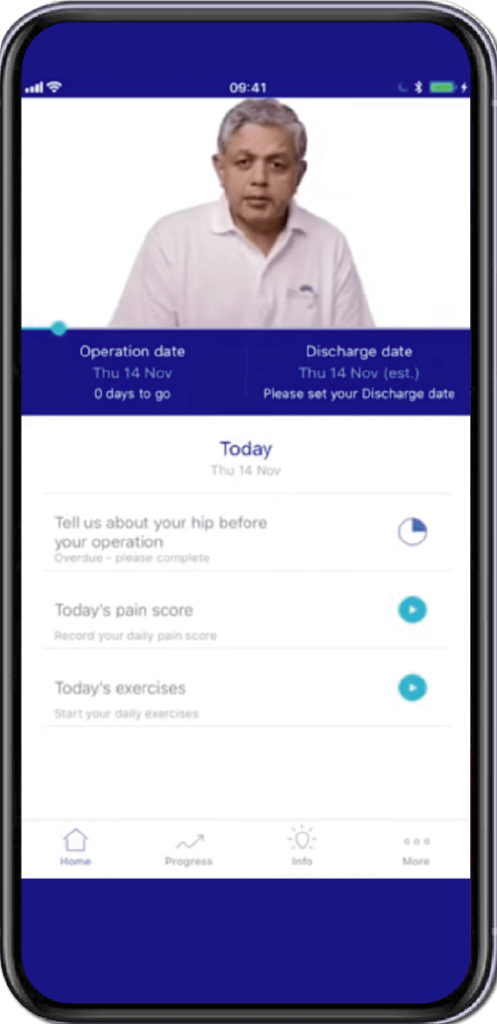
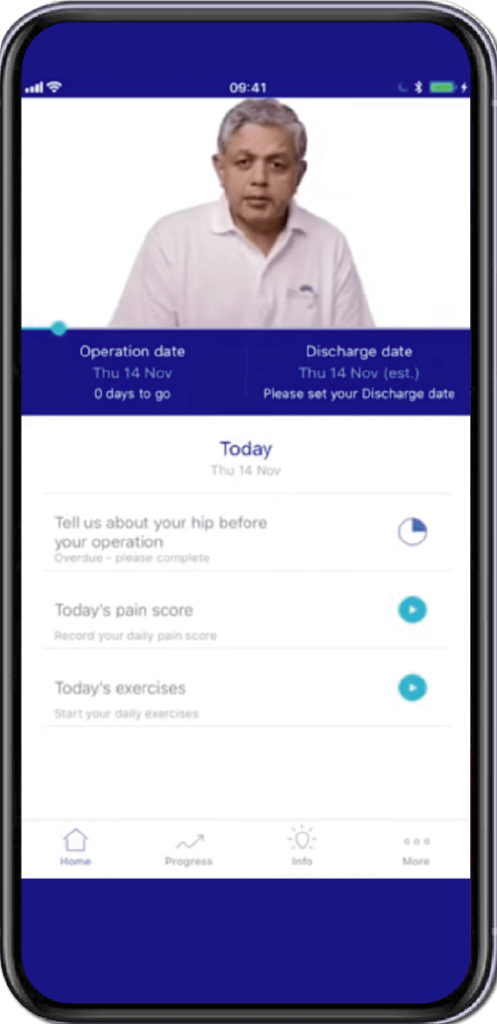
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
