
Osteoporosis
Osteoporosis is a common degenerative bone disease resulting from reduced bone density. Osteoporosis is not a painful condition unless there is a fracture. People affected by osteoporosis are at an increased risk of fractures, especially of the hip, spine, and wrist.
What is Osteoporosis?
Osteoporosis is a common degenerative bone disease resulting from reduced bone density and strength. Osteoporosis is not a painful condition unless there is a fracture. People affected by osteoporosis are at an increased risk of fractures, especially of the hip, spine, and wrist.
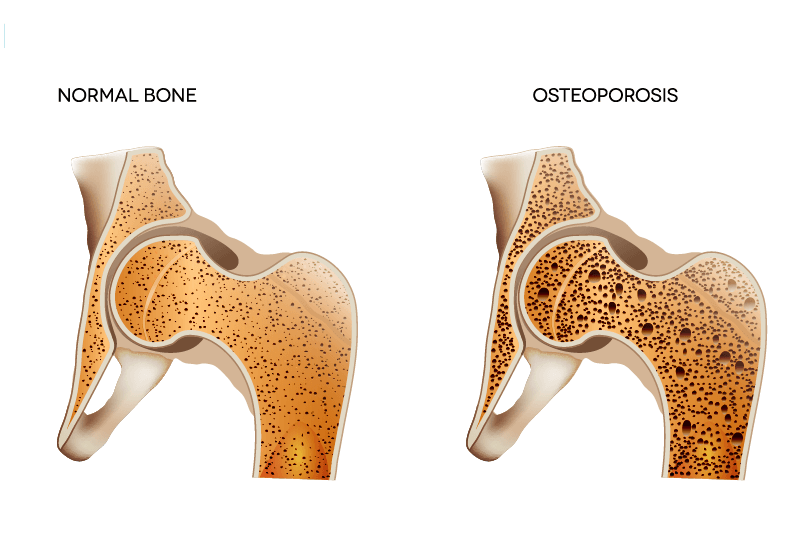
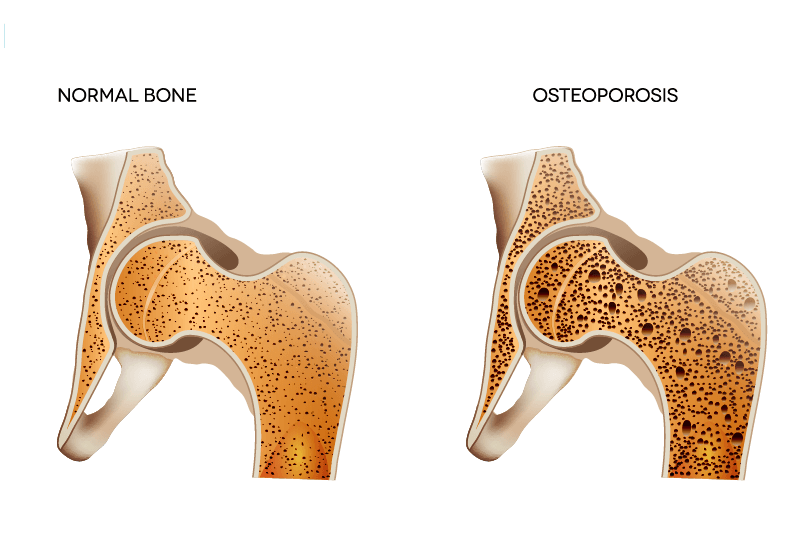
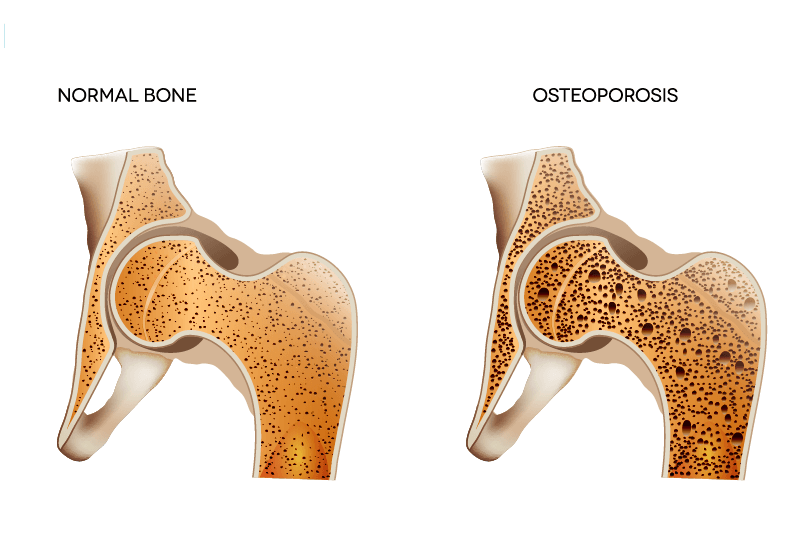
Bone consists of living tissue which is continuously being broken down and renewed. Osteoporosis occurs when the speed of creating new bone cannot keep up with the loss of old bone. Osteoporosis means “porous bone.” Healthy bone has a honeycomb structure when viewed under a microscope. In osteoporosis, these spaces in the bone structure are much larger than in healthy bone structure. As bones become less dense, they become weak and are more likely to break. People above 50 who have had a fracture following a fall from standing height must ask their family doctor about a bone density test.
Osteoporosis affects people of all races. Asian and white post-menopausal women are at the highest risk. Medications, a healthy diet and regular strength and weight-bearing exercise can help prevent osteoporosis.
How the body and bones change with Osteoporosis
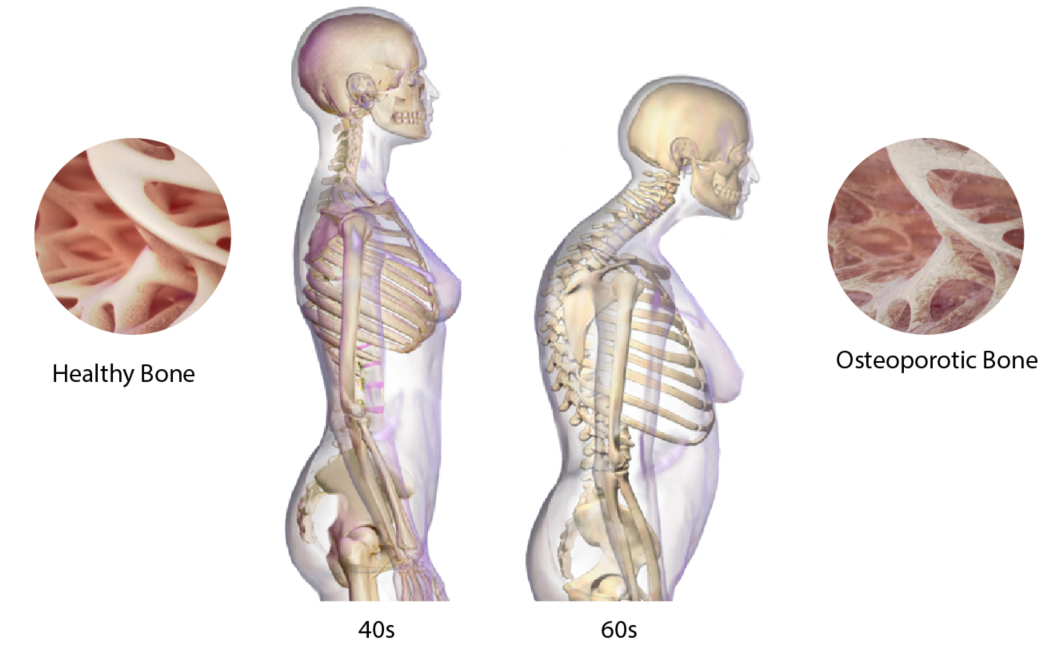
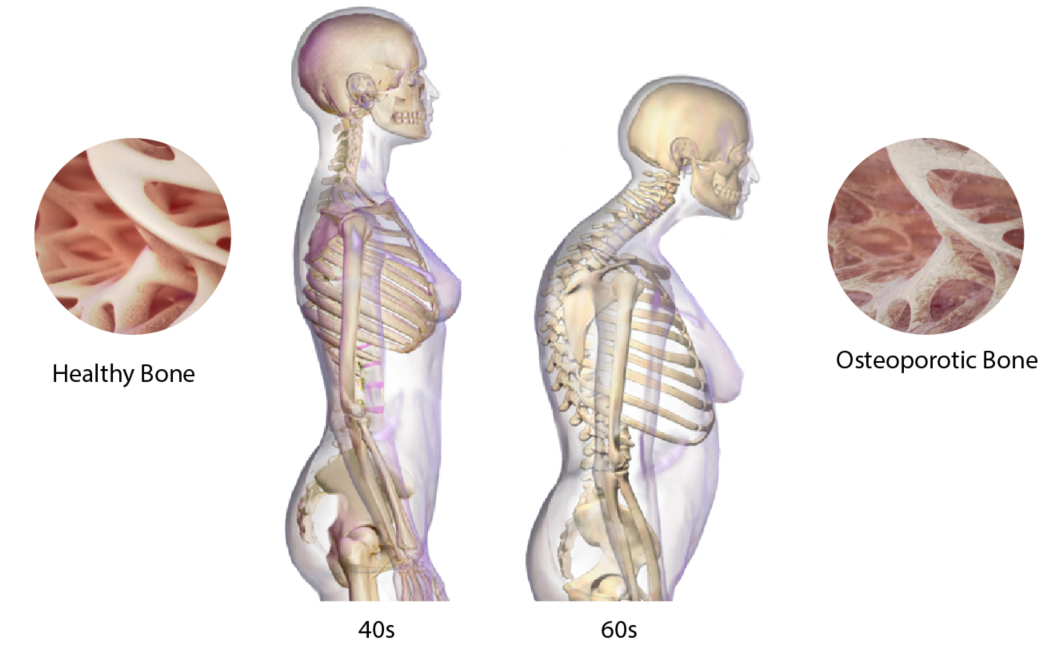
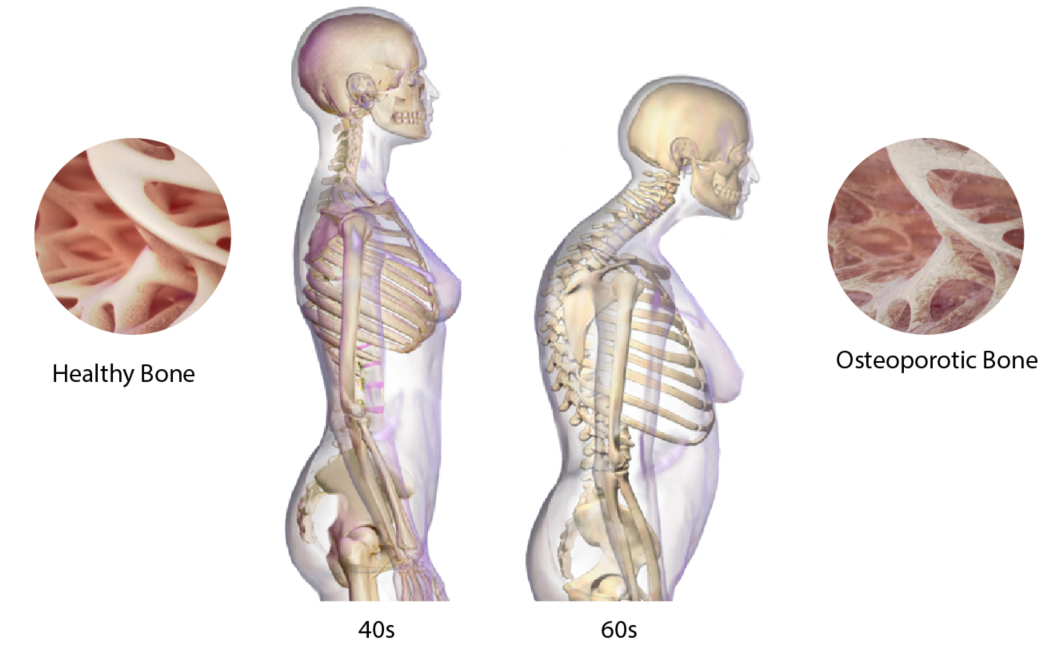
HOW OSTEOPROSIS AFFECTS THE SPINE OVER TIME
What are the symptoms of osteoporosis?
Early stages of Osteoporosis usually show no symptoms making it difficult to diagnose. If early-stage symptoms do appear at all, they may include:
- receding gums
- weakened grip strength
- weak and brittle nails
What happens when osteoporosis is severe?
Once bones lose density and are weakened by the disease, signs and symptoms include:
- Back pain, caused by a fractured vertebra, resulting in a hunched posture
- Reduction of height over time
- Bones that are more fragile than normal
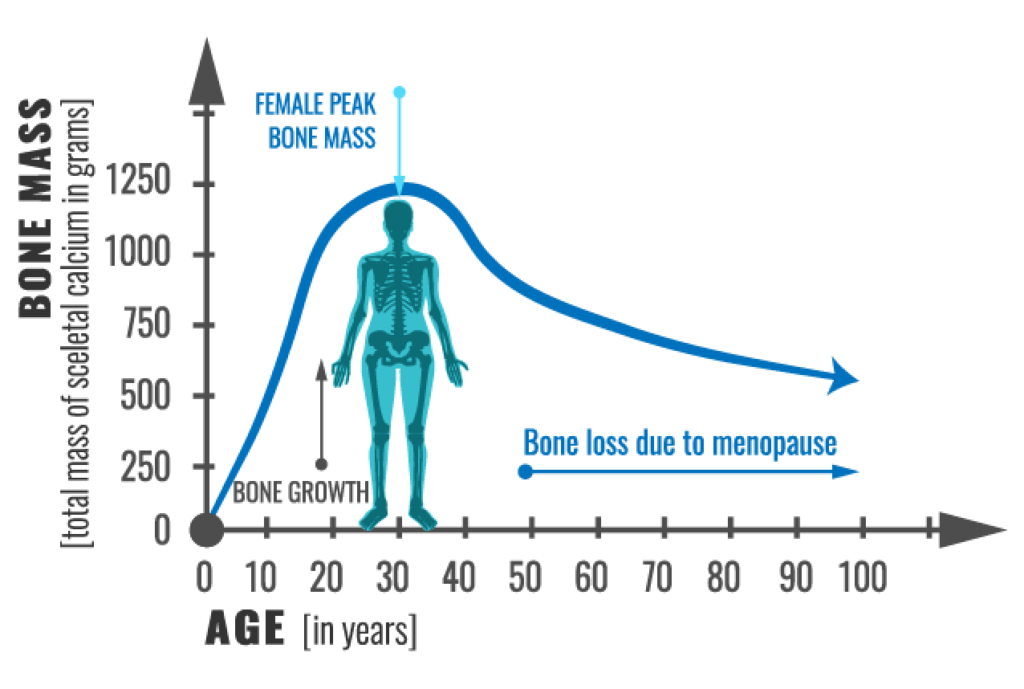
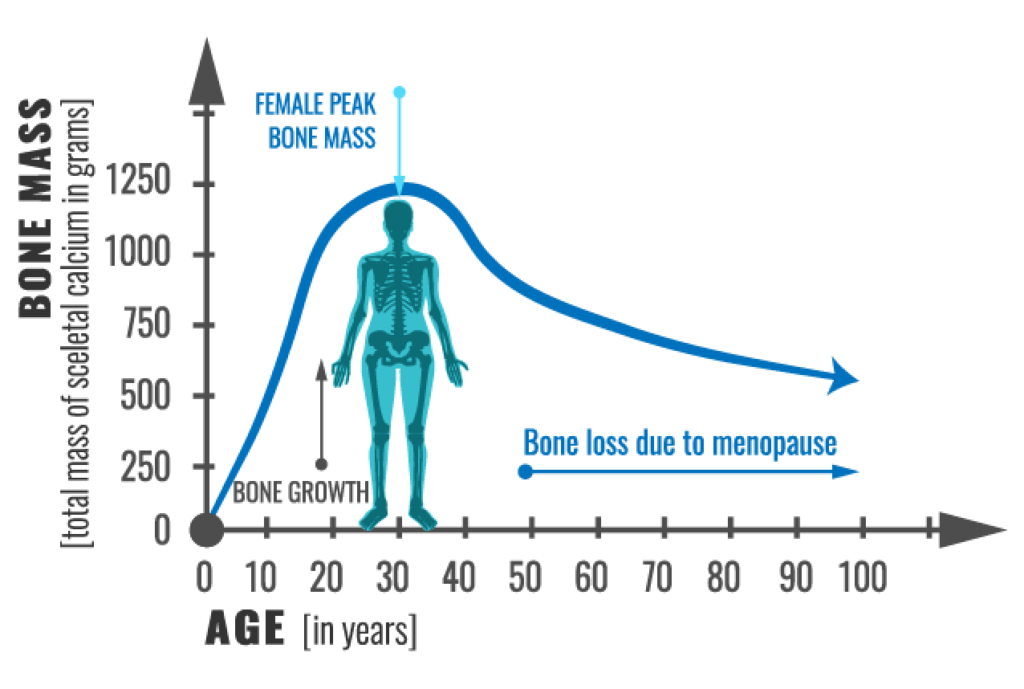
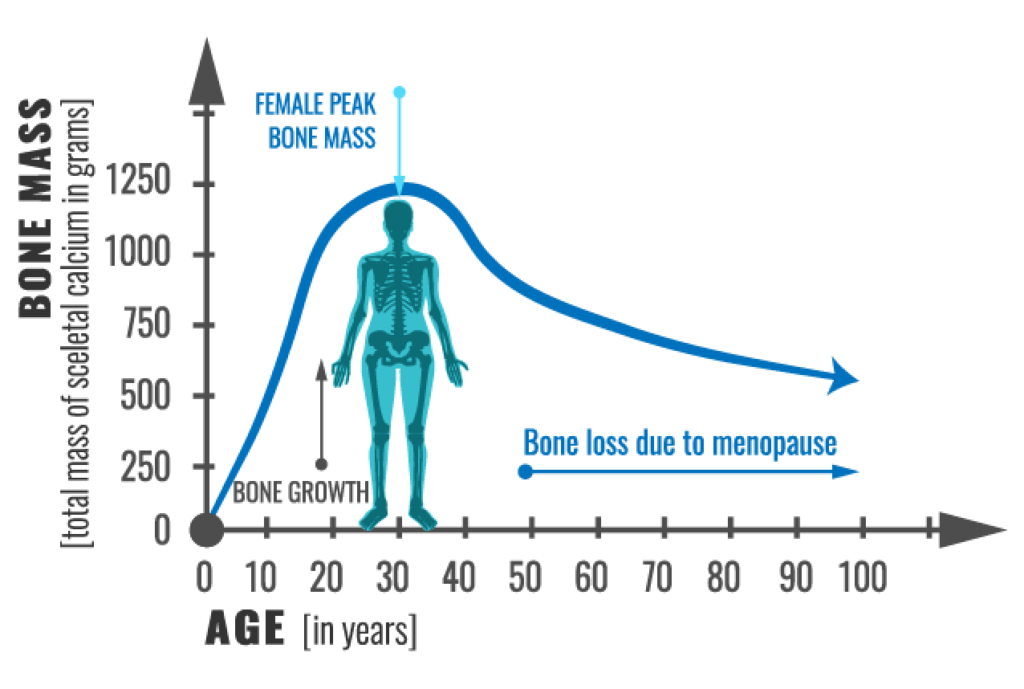
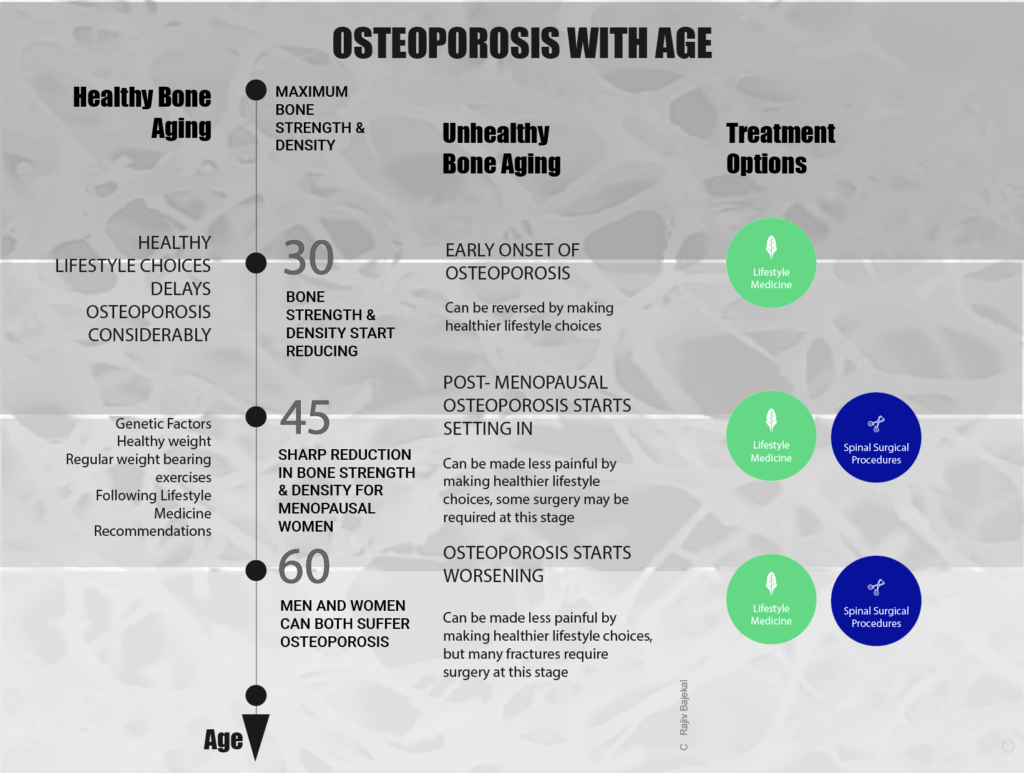
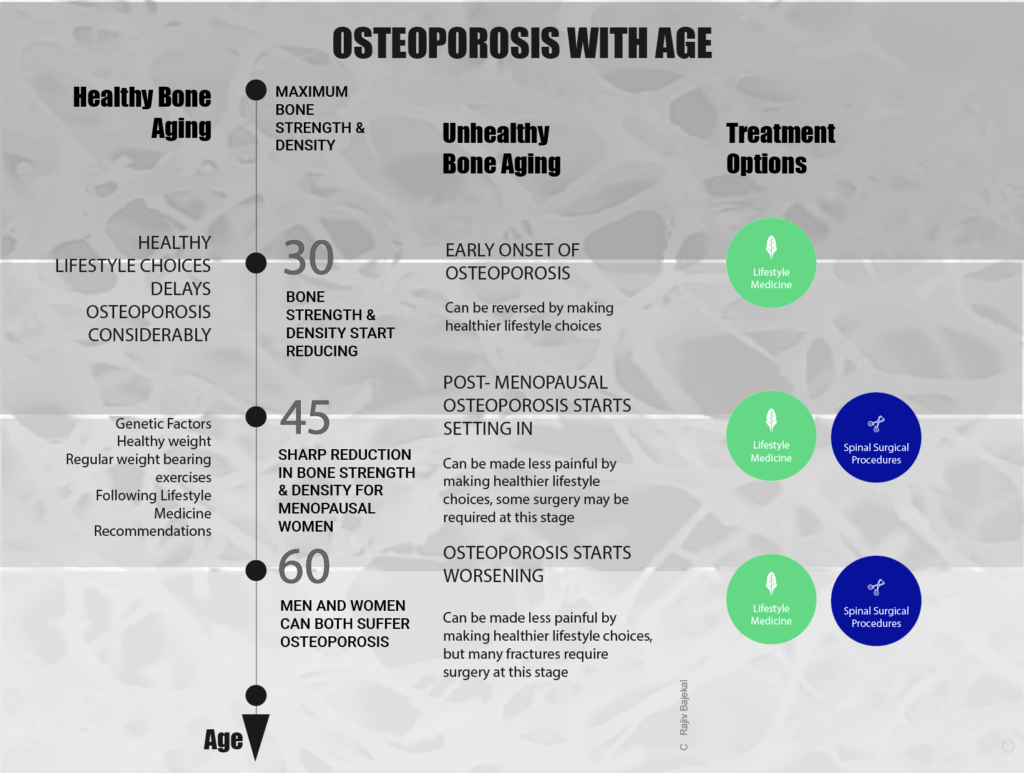
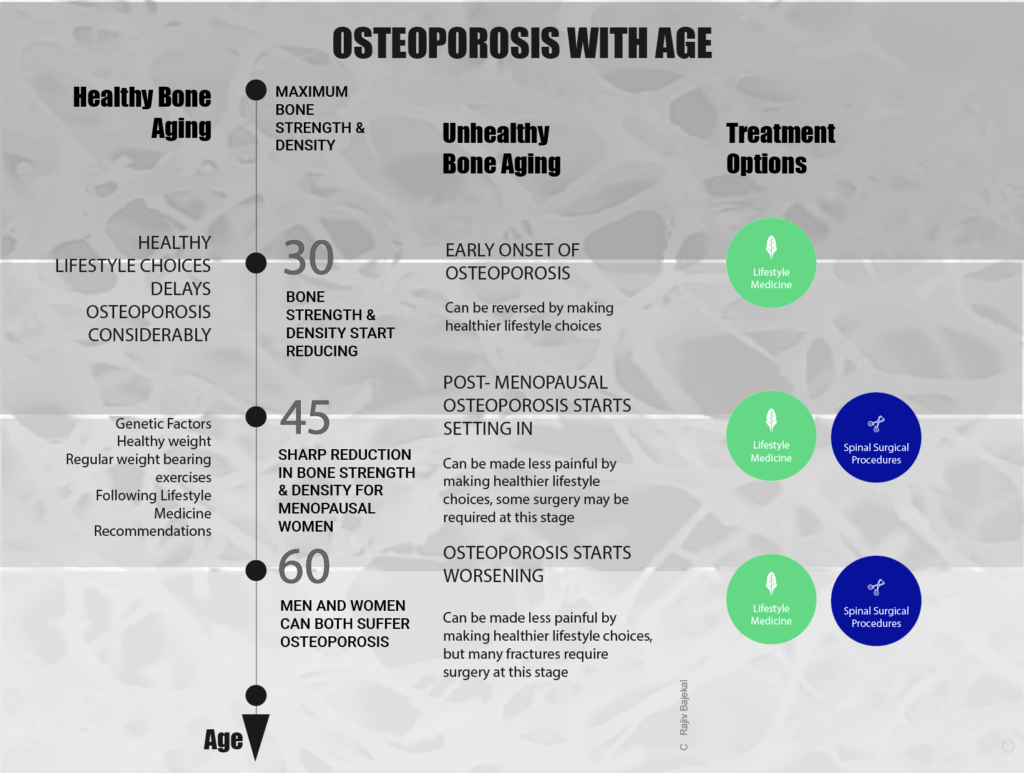
Human bone tissue is constantly renewing itself, rapidly during youth but slowing down after the 20’s peaking at the age of 30. After 30, the rate of bone mass reduction is more rapid than bone tissue replacement, reducing further as we age.
With progressing age, osteoporosis can result in compression fractures in the spine stooped posture and height loss, and sudden back pain. It is best to improve one’s lifestyle to prevent osteoporosis or at least delay its onset.
OSTEOPOROSIS
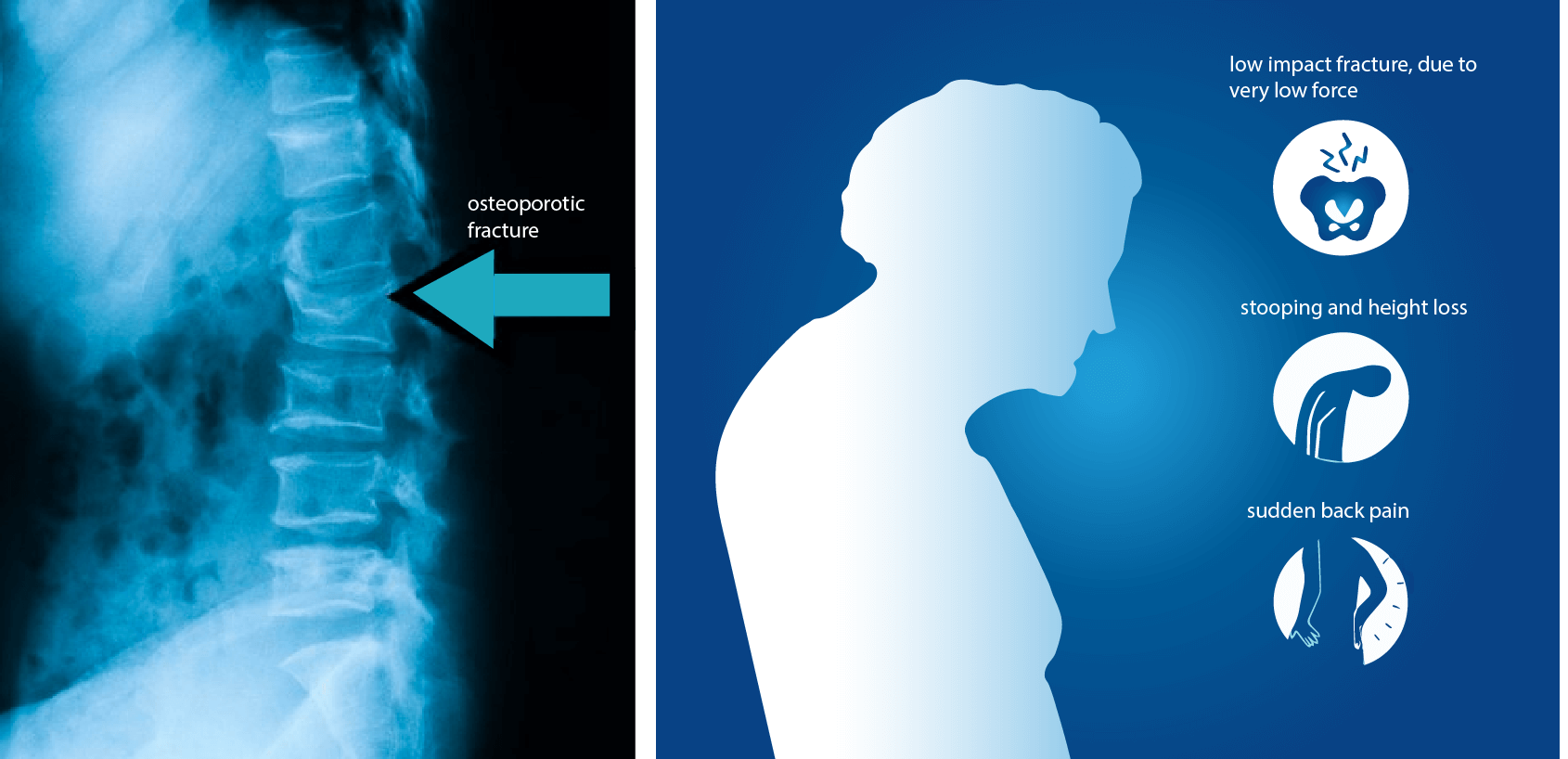
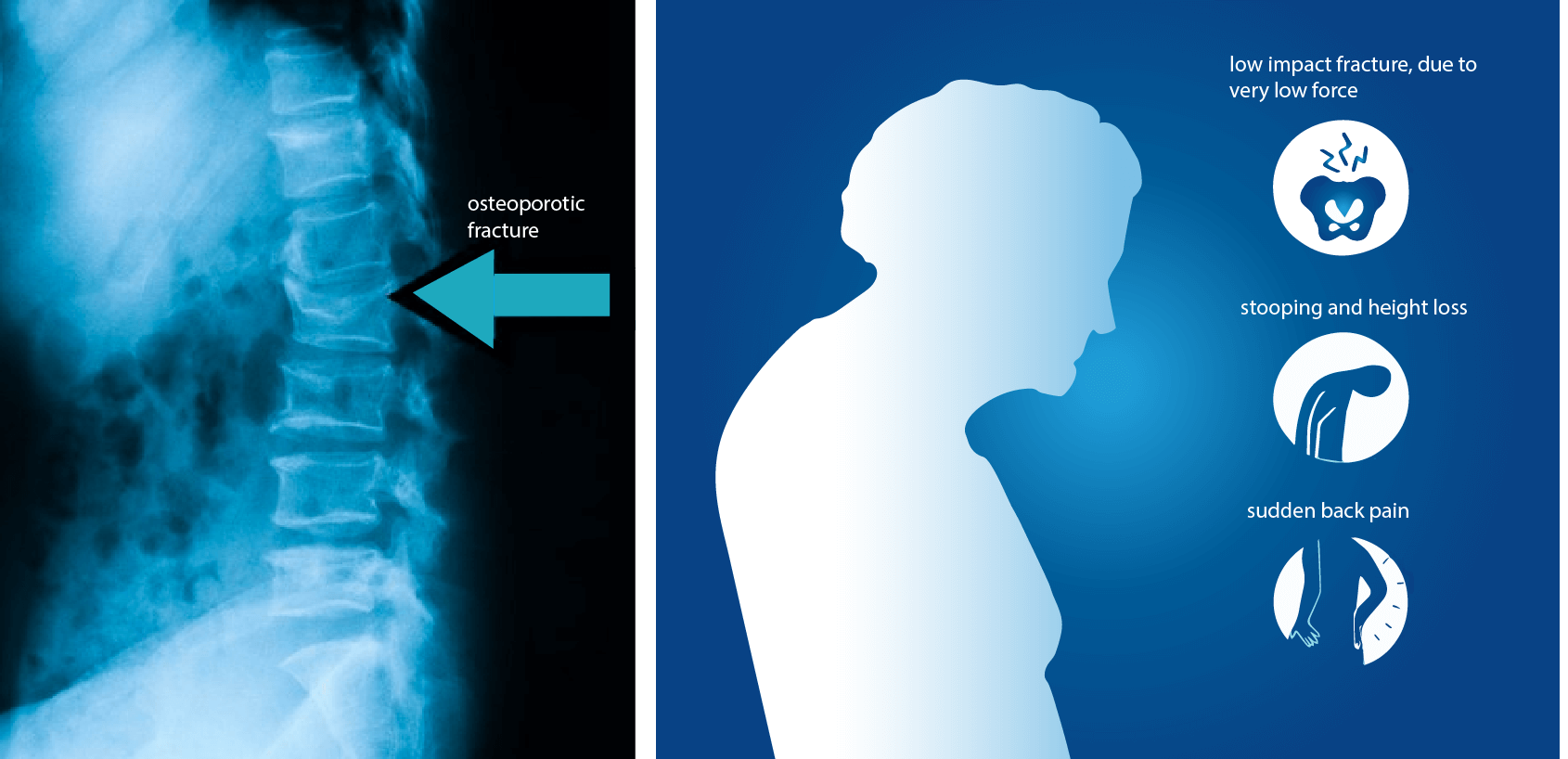
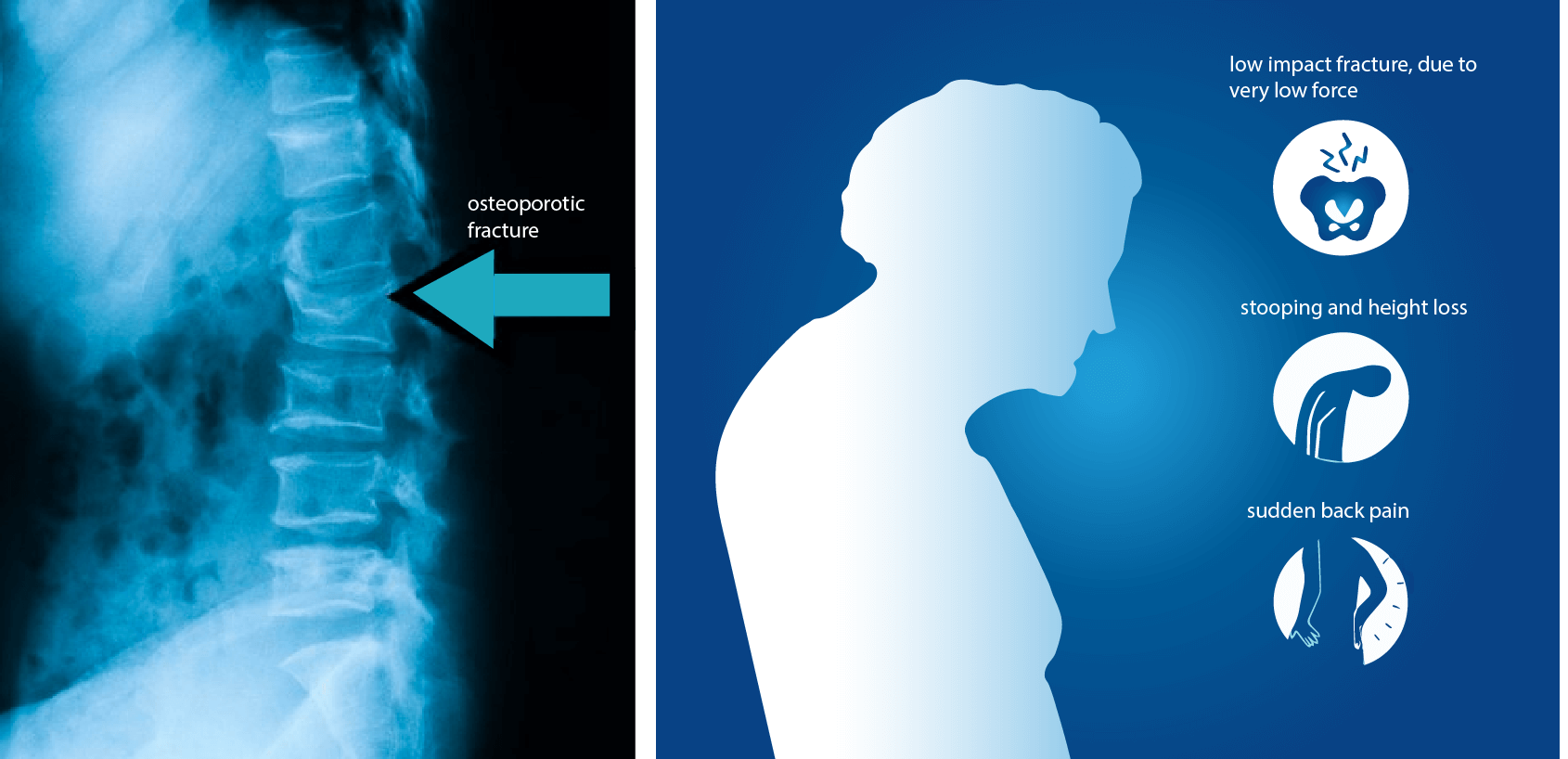
With progressing age, osteoporosis can result in compression fractures in the spine resulting in stooped posture and height loss, and sudden back pain. It is best to improve one’s lifestyle to prevent osteoporosis or at least delay its onset.
What Are The Risk Factors For Osteoporosis?
An individual’s likelihood to develop osteoporosis depends on various factors, including genetics and an individual’s bone mass before 30. Bone mass density is inherited somewhat and varies by ethnicity. Higher peak bone mass at 30 lowers the likelihood that one will develop osteoporosis with ageing.
Significant risk factors for osteoporosis include the following:
- Gender – females are more prone to osteoporosis
- Age – Osteoporosis is very frequent in elder people
- Menopause – Hormonal changes during menopause leads to rapid loss of bone density in
women. - Ethnicity- being Caucasian or Asian increases likelihood of osteoporosis
- Genetics – family history of osteoporosis
- Poor nutrition
- Physical inactivity
- Tobacco and smoking
- Low body weight and small-boned frame
Whereas one can control some of the risk factors for osteoporosis, such as lifestyle, there are others such as genetics and gender are impossible to control.
BONE POROSITY IN
OSTEOPOROSIS
DECREASING BONE MASS
WITH AGE IN WOMEN
How do I prevent Osteoporosis?
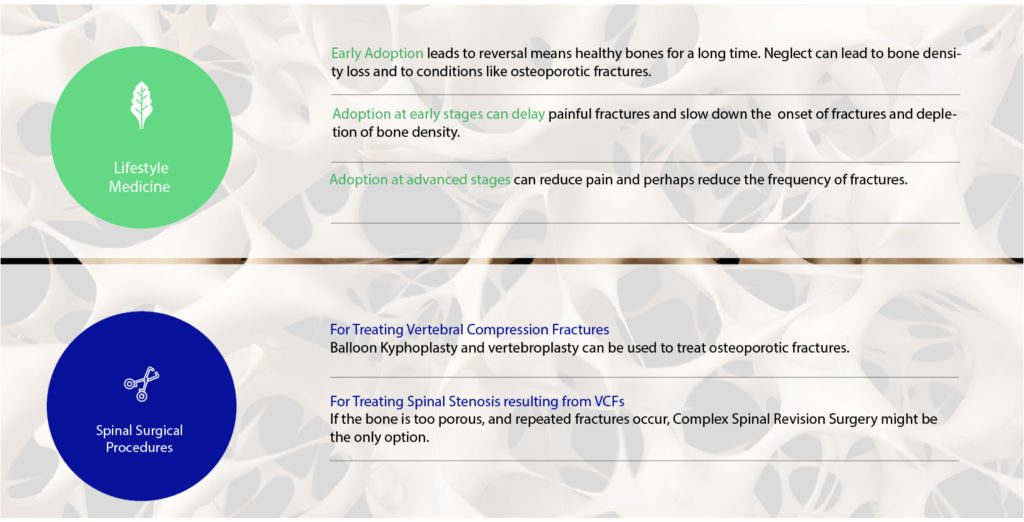
Onset of osteoporosis can often be delayed or prevented by following a healthy lifestyle and maintaining a healthy body weight. Lifestyle medicine changes can help turn around poor nutrition, tobacco usage and inactivity. For instance, you can improve your diet and start an exercise program to benefit bone health. If neglected, osteoporosis can become more acute, needing medical intervention to reduce the impact of this painful debilitating disease. A good mix of weight bearing exercises such as skipping, running, weight training (resistance exercises), walking with weighted jackets and wrist bands plus improving balance and coordination by Tai-chi can prevent falls and lower risks of sustaining fractures. Even if you have been diagnosed to have severe osteoporosis, there is a role for changes in lifestyle to strengthen your bones.
SOLUTIONS & TREATMENT OPTIONS FOR OSTEOPOROSIS
When might treatment for osteoporosis be required?
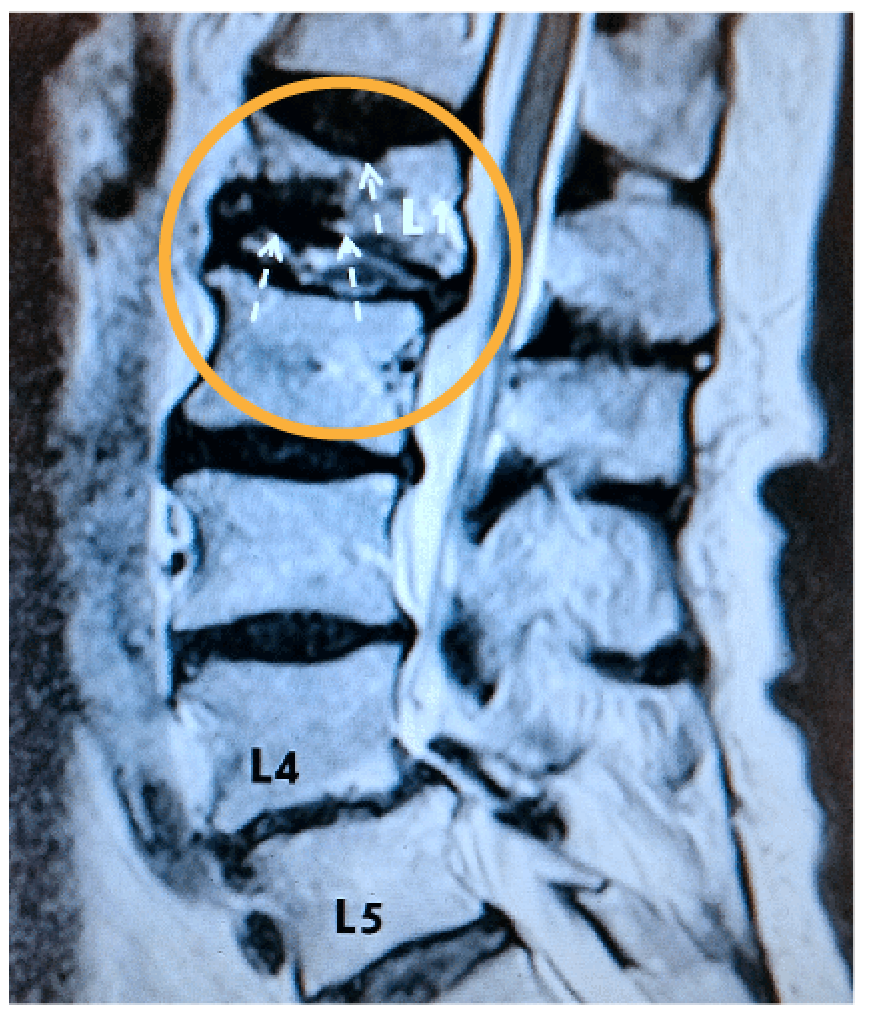
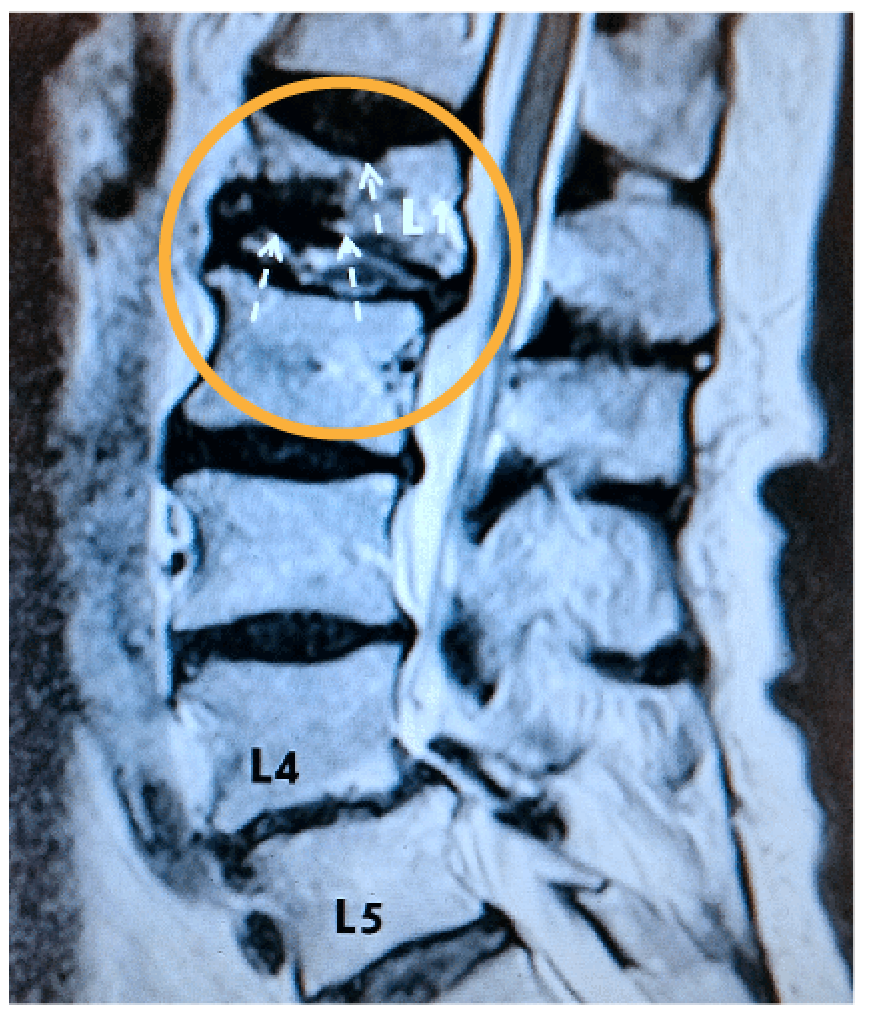
In severe cases of osteoporosis, medical intervention becomes necessary. Unfortunately for most, since early onset is symptomless, the first time their spinal osteoporosis is diagnosed is with a vertebral compression fracture. The tell-tale symptom is the stooped posture which occurs due to vertebral collapse resulting in pain.
How is osteoporosis diagnosed?
I may suggest x-rays, computed tomography (C.T.) or a magnetic resonance imaging (MRI) to confirm the diagnosis of osteoporosis. This would help to predict the prognosis and determine the best treatment option for you going forward.
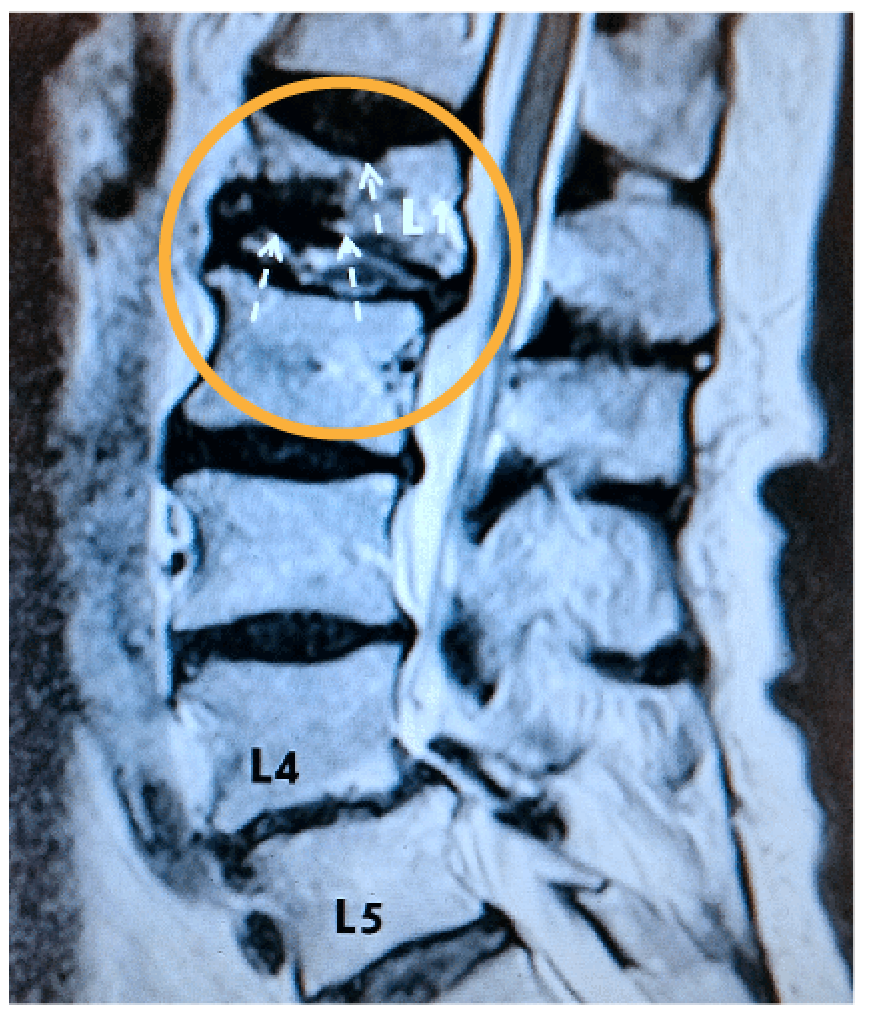
How is Osteoporosis diagnosed?
Osteoporosis is best diagnosed by a DEXA scan. I may suggest x-rays, computed tomography (CT Scan) or a magnetic resonance imaging (MRI) to confirm the diagnosis of an osteoporotic fracture of the spine.
How Is Osteoporosis Treated?
Osteoporosis is managed with lifestyle changes which include a mix of exercises such as resistance training and weight bearing exercises, but if it is severe and there is a risk of fractures or if you have already had a fracture, medication which slows down bone resorption may be of benefit to you. Remember that lifestyle changes are beneficial at all stages of osteoporosis and the use of medication does not mean that other aspects should be ignored.
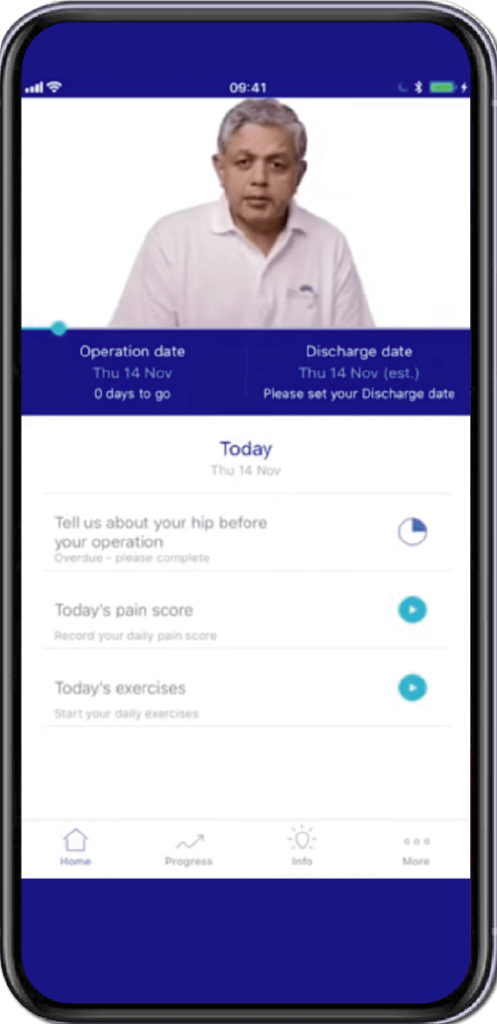
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
