
SPINAL FUSION
When stenosis has resulted in forward slippage of a vertebra or curvature of the spine, patients may require spinal fusion surgery. Two or more vertebrae are fused permanently in this procedure, using a bone graft from bone removed during decompression surgery.
When would I need a Spinal fusion?
Most people with a symptomatic lumbar spinal stenosis usually require just a spinal decompression spinal decompression lumbar laminectomy to relieve pressure on the nerves. However, if stenosis has resulted from forward slippage of a vertebra or curvature of the spine, you may require spinal fusion surgery. Two or more vertebrae are fused permanently in this procedure, using a bone graft from bone removed during decompression surgery.
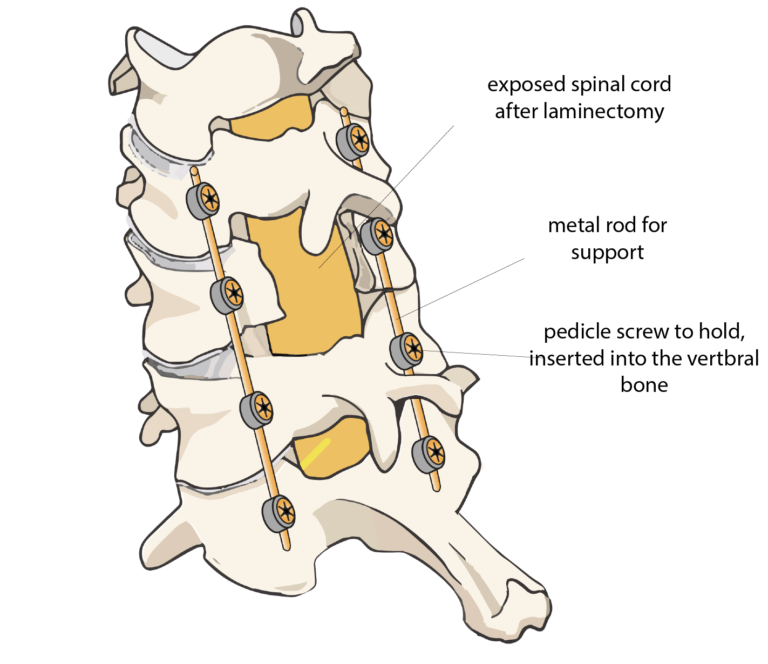
By fusing your vertebrae, the movement between the vertebrae is reduced. It also helps prevent worsening of the spinal curvature or slippage after surgery, which can cause more back or leg pain. I may use screws and rods to hold the spine in place while the bones fuse. The use of rods and screws speeds the fusion process as well as post-operative recovery in some situations. Overall, the results of spinal fusion are good to excellent in approximately 8 out of 10 when used for this indication, with more improvement in leg pain than back pain. Most people can resume a normal lifestyle after a period of recovery from surgery.
I will discuss all benefits and risks of the procedure with you at your consultation. If you have any concerns about the procedure please ask me during your consultation. I work with a team of three consultant surgeons, a consultant radiologist, and a very experienced physiotherapy team and discuss all complex cases in our fortnightly multidisciplinary team meeting to be able to provide a first-class service.
What happens in a Spinal Fusion Surgery?
When the pain from a spinal stenosis cannot be resolved by conventional means, a spinal fusion operation can help. A laminectomy is carried out to reduce the pressure on the spinal cord, after which the bones of the vertebrae are fused using screws and rods, to ensure to prevent worsening of the spinal curvature.
Getting ready for surgery
There are risks of an anaesthetic and surgery, such as developing pneumonia etc. Elderly people have higher rates of complications from surgery. So do people with excess weight or medical illnesses such as Type 2 diabetes, heart disease, if you smoke or if you have multiple medical problems.
You must inform my anaesthetist, the nurse looking after you, preassessment team and me of all the medications you are taking, any allergies that you may have including drug reactions as these can seriously impact your surgery and recovery. Drugs such as aspirin, clopidogrel, and other blood thinners may need to be reviewed or stopped under guidance before surgery. If you are diabetic, especially on insulin, this needs to be highlighted early.
Do try if time permits to stop smoking, lose weight and make some lifestyle changes as these will make your recovery smoother.
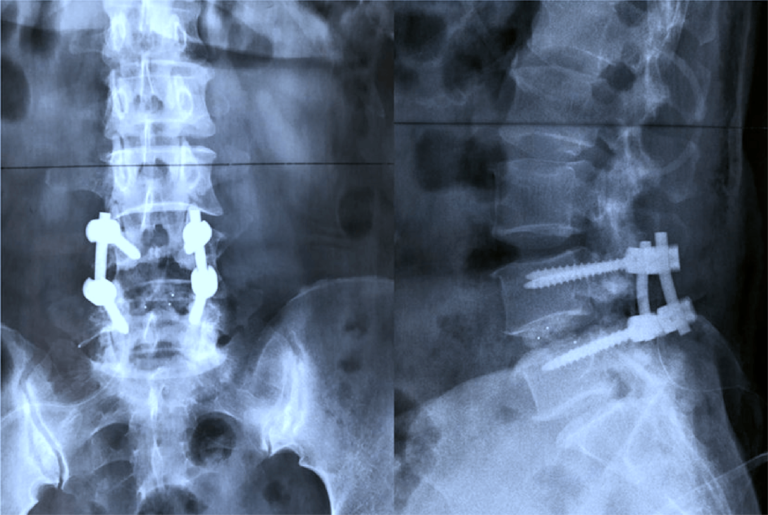
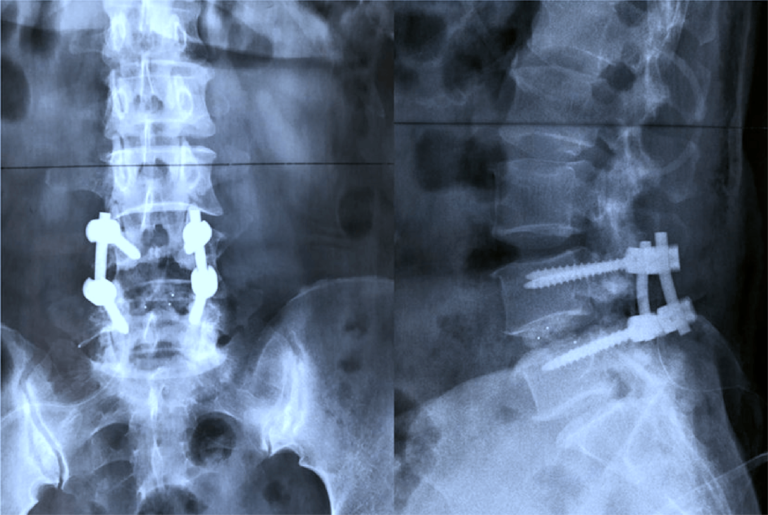
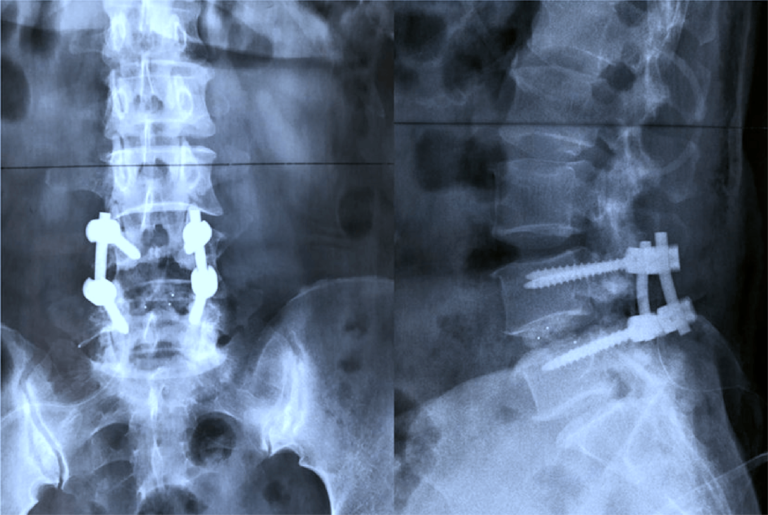
X-ray of a Spinal Fusion
Note the screws and rods around the spine in the adjacent x-rays. The laminectomy is clearly seen on the vertebral bone in the first image.
The additional support from the screws and rods helps the bones to fuse and heal faster than otherwise.
What are the risks of spinal fusion surgery?
- Bleeding
- Infection
- Blood clots
- Spinal nerve root injury
- Spinal fluid leak as the surgery is close to the thin membranous lining of the nerves (dura).
- Infection: The risk of infection is less than 1%. All my patients receive a dose of intravenous antibiotics when they are going off to sleep. If you develop an infection, it is most likely to be a superficial wound infection that will resolve with a short course of oral antibiotics and not a cause for serious concern.
- Bleeding: Blood loss is usually minimal with a laminectomy.
- DVT: Developing blood clots in the legs (deep vein thrombosis – DVT) is a risk of any surgery. The risk is minimised by using thrombo-embolic deterrent stockings (TEDS) and mechanical pumps. These pumps squeeze your lower legs, helping the blood to circulate. They are put on when you go to sleep and stay on until you start to mobilise. I encourage early mobilisation as this also helps to prevent DVT.
- Nerve Injury: Nerves are compressed by ligament and bone and are often adherent to the nerves which can be physically damaged at the time of surgery when separating and removing the ligaments and bone from the nerves. This can lead to a loss of nerve function with persisting pain, weakness and numbness in the territory of that nerve. I keep this risk to a minimum by using magnification and careful dissection around the nerves.
- Dural Tear: Rarely there can be an injury to the thin membrane that surrounds the nerves (Dural tear) which can result in a CSF leak. This can usually be repaired at the time but sometimes needs another operation to address it.
What are the long term risks?
About 20 % of patients may not benefit from surgery, especially in cases of long-term nerve compression. Patients having very severely compressed nerves are at a higher risk of nerve damages or, more commonly, a CSF leak where the fluid surrounding the nerves and enclosed in a thin membrane leaks out. This can be repaired at the time, though you may require further surgery to prevent re-leaking. More neurologically severe complications, like complete paralysis, are rare. Rarely, misplacement of the screw may cause nerve damage needing revision surgery.
This type of surgery is not suitable for all patients and I will guide you with all available options and give you my own higher success rates.
How long should I expect to stay in hospital?
The procedure involves a hospital stay of one to four days following a spinal fusion surgery.
What can I expect after my surgery?
Pain medication is administered initially through an intravenous (IV) line, followed by oral pain-relieving medications to keep you comfortable.
You are encouraged to move, usually the following day. You should get out of bed with assistance and sit on a chair. This helps to retain muscle tone and prevent immobilisation. Walking is encouraged as it strengthens the lower back and leg muscles and helps in surgical recovery. Next, walking on stairs is introduced and you will be assisted by a physiotherapist.
The incision area may have a bulky dressing that is changed to a waterproof dressing the day after surgery.
I recommend that you avoid driving, excessive sitting, lifting, or bending down for about a month after surgery. Be guided regarding how much you move or bend in the first few weeks after surgery based on your pain. If it is painful, be careful of overdoing it. Your physiotherapist will demonstrate exercises to strengthen the back and to prevent scar formation around the nerve.
Following a hospital stay, you are given a physiotherapy program before discharge to help recover.
What should I expect at home?
- The treating physiotherapist usually provides exercises that you can follow easily at home. The ward team will prescribe pain-relief medicines. Non-steroidal anti-inflammatory drugs (NSAIDs) are not always prescribed as they can cause oozing from the wound.
- Stool-softeners. These are sometimes required initially to in to avoid constipation which would prevent excessive straining during bowel movement.
- Look after your wound by avoiding activities like bathing, swimming, and hot-tubs until the incision has completely healed to prevent rupturing of sutures and infection from setting in. The absorbable sutures used for surgery usually dissolve in a few days after surgery. A water proof dressing is used to cover the wound to allow showering. Do ring the ward if you have any concerns.
- You should continue with the physiotherapy program and follow the prescribed exercises. You should avoid activities like running or lifting heavy weights (typically over 5 pounds).
- You are advised to use compression stockings to prevent blood clot formation, until you are completely mobile.
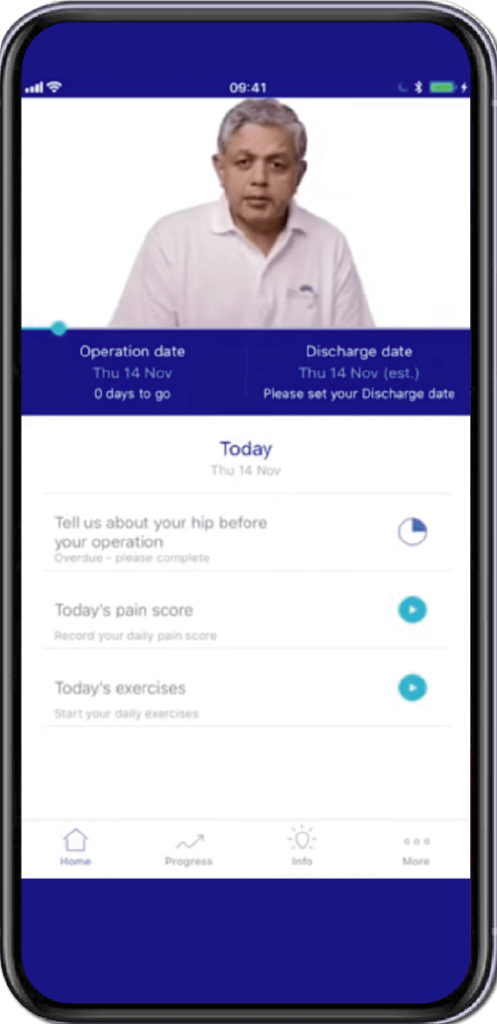
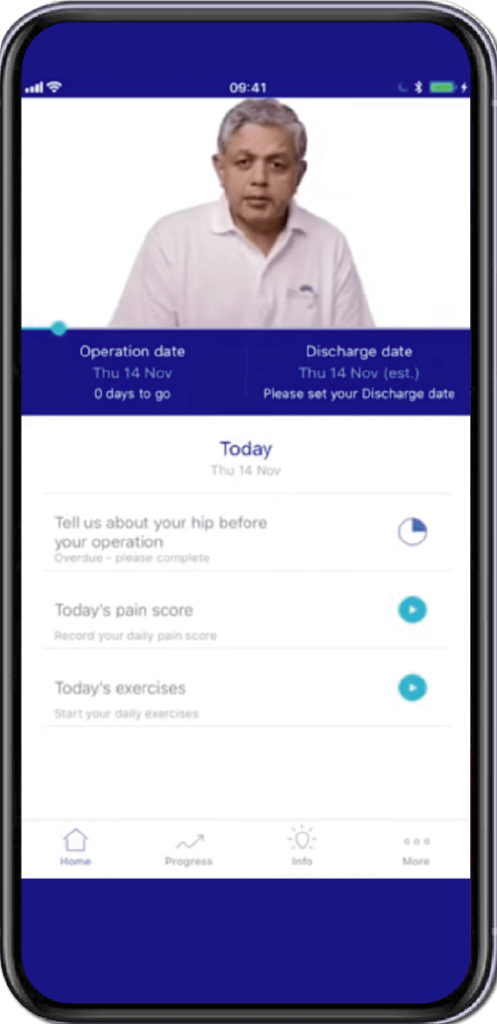
- I would like you to download and use the link to the app for MyRecovery to collect information which helps me improve my service (https://www.myrecovery.app/rba)
What is the expected recovery time from this operation?
You will generally return to normal activities in 2 to 3 months.
How to do I prevent Spinal Stenosis and recurrence after surgery?
The best way to avoid lumbar spinal stenosis is to stay as physically fit as possible. Regular exercise can improve endurance and keep the muscles that support the spine strong. Avoiding weight gain can decrease the load that the lumbar spine must carry. You should avoid cigarette smoking. Both the smoke and the nicotine cause the spine to degenerate faster than normal.
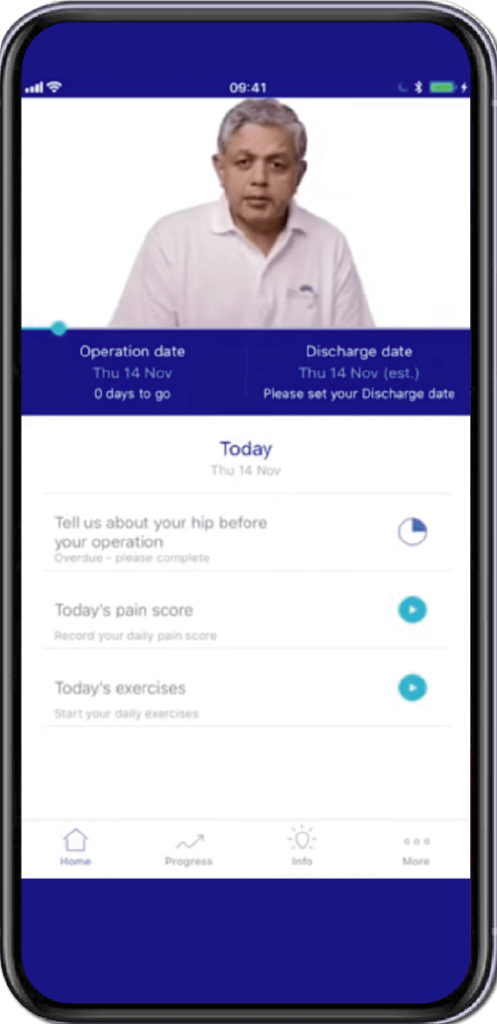
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
