
Spinal stenosis
Spinal stenosis is the narrowing of the spinal canal, leading to additional pressure exerted on the spinal nerves as they exit the spine and branch out to the muscles.
What is Spinal Stenosis?
Spinal stenosis is the narrowing of the spinal canal, leading to additional pressure exerted on the spinal nerves as they exit the spine and branch out to the muscles. Stenosis means narrowing. It is a degenerative condition seen most commonly in people above 60 years, though it may occur in younger people. Spinal stenosis can happen in any part of your spine but is most common in the lower back or lumbar region.
What are the typical symptoms of spinal stenosis?
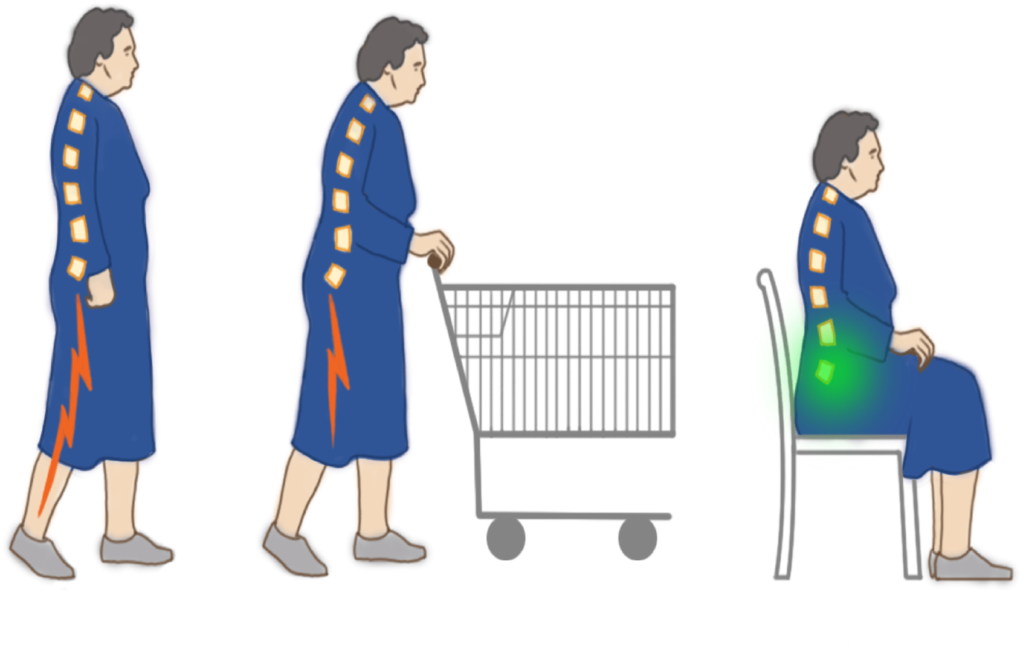
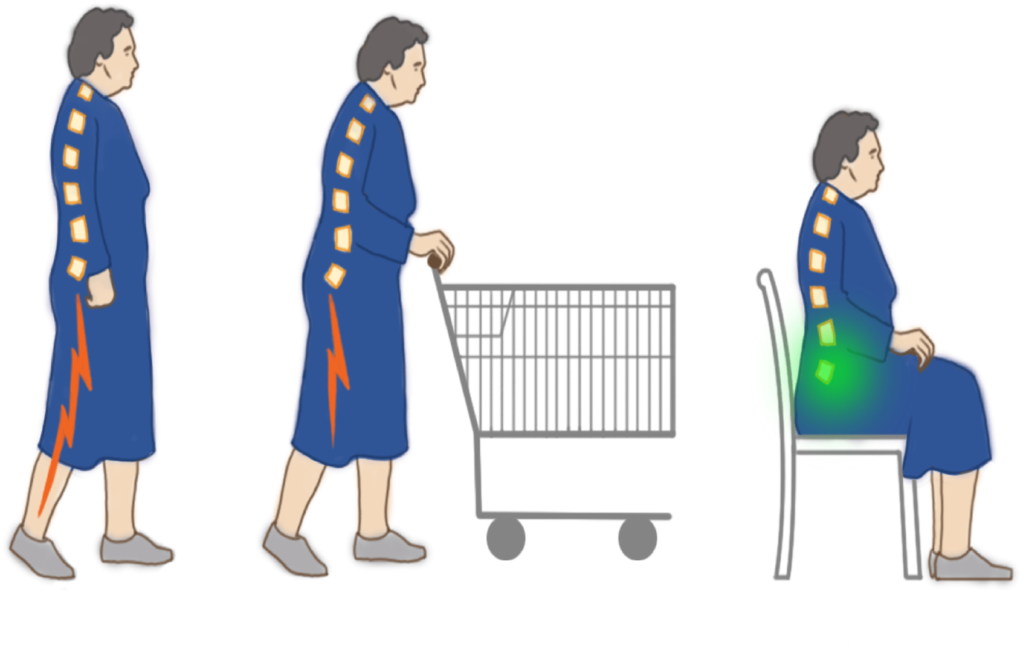
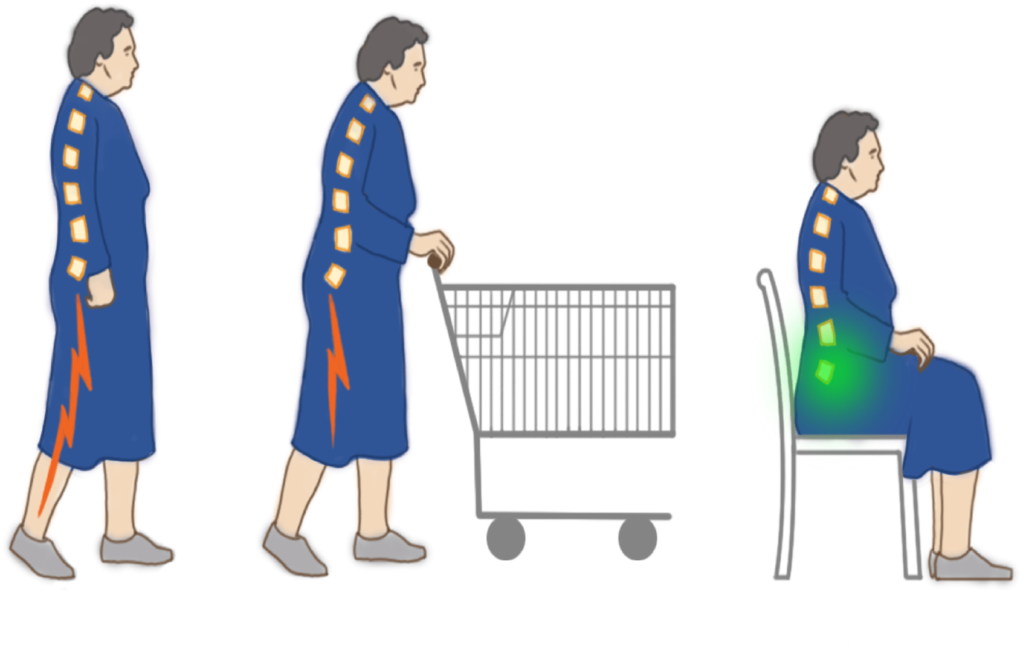
Virtually all individuals in their seventies show at least some degree of spinal stenosis on imaging studies. Only a fraction manifest the actual symptoms of central and foraminal stenosis. Typically, patients with lumbar spinal stenosis have a long history of pain in the back and buttocks, sometimes including the legs, that gradually worsen. Standing or walking upright usually increases the symptoms, resulting in an achy pain, tightness, heaviness, and a sense of weakness in the buttocks and legs, often called spinal claudication. These symptoms are generally relieved by sitting down or leaning forward, increasing the space around the nerves.
Although patients with lumbar spinal stenosis cannot walk for long periods, they may ride an exercise bicycle for much longer. Some patients also find that it is easier to walk while leaning forward on a shopping cart. This position tends to increase the space in the spinal canal, which tends to alleviate the pressure exerted on the nerves. Leaning forward on the handlebars of a bicycle creates the same effect. Spinal stenosis may cause instability or difficulty with balance and even urinary symptoms.
Though spinal stenosis patients typically experience pain along a nerve on the side of the leg, their pain reduces on resting or leaning forward. A physical examination can be inconclusive in patients with spinal stenosis. It is essential to make sure the patient does not have underlying vascular problems and rule out associated hip problems that can give rise to similar symptoms.
Typical Symptoms of Stenosis
Typically, those suffering from stenosis find it easier to lean forward or sit because it alleviates the pressure on the nerves and tends to create more space in the spinal canal.
What causes spinal stenosis?
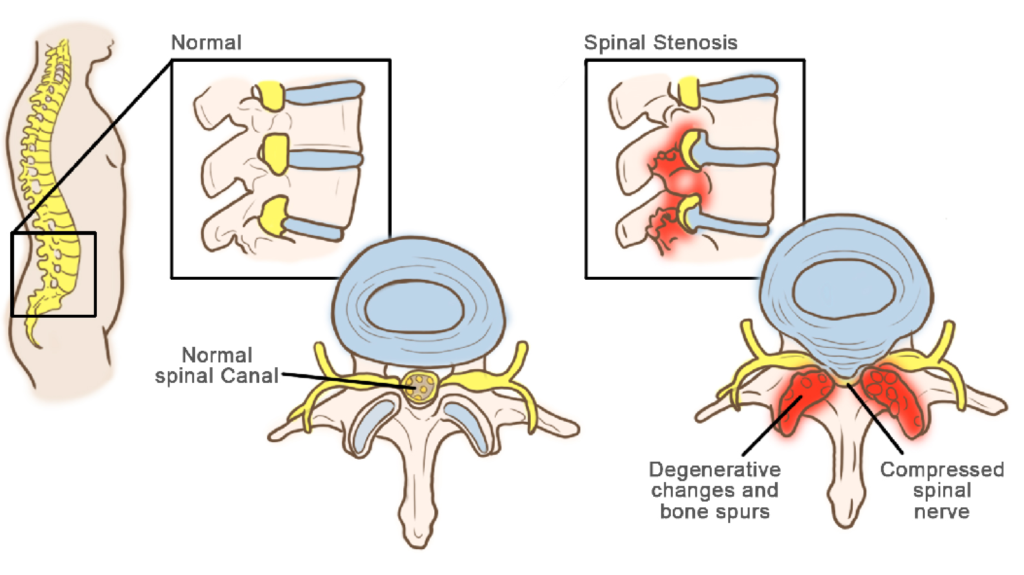
The cause of the narrowing of the central canal and the intervertebral foramina is due to a bulging disc, enlargement of the facet joints or simply thickening of ligaments. Trauma, spinal fractures, or previous spinal surgery can result in temporary constriction of the spinal canal, causing spinal stenosis.
Why does it happen?
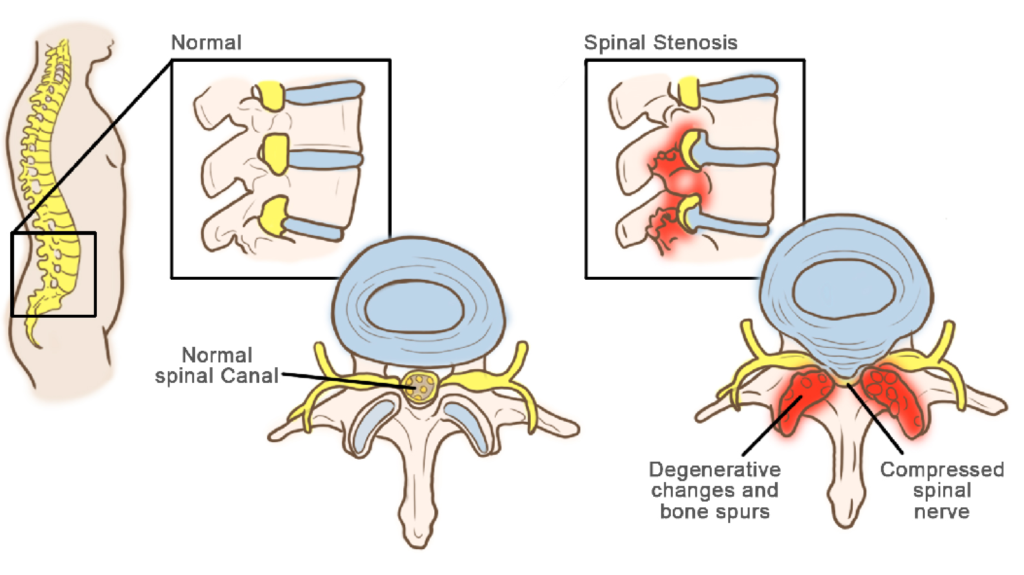
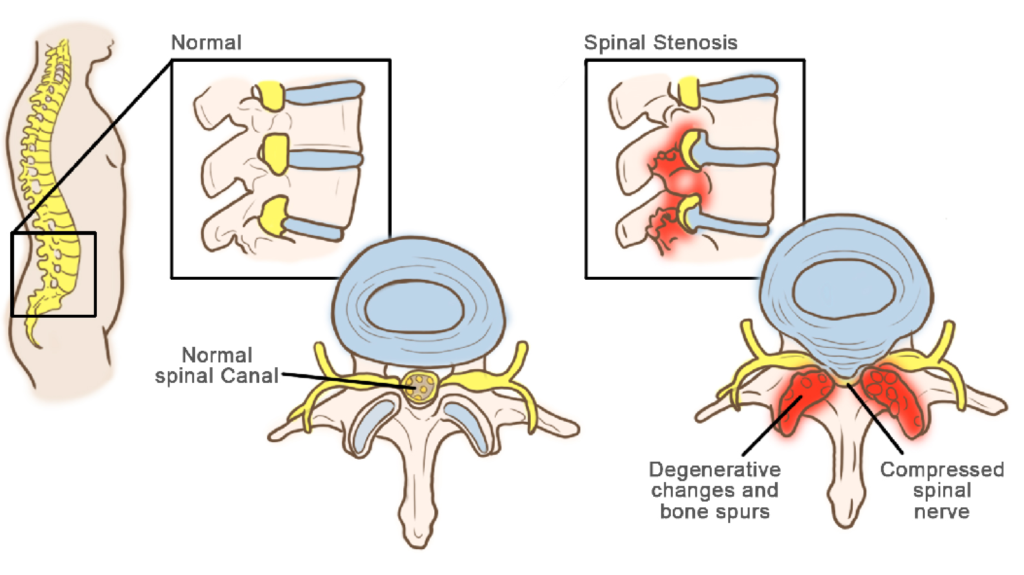
Spinal stenosis is a painful spinal condition due to the degeneration of the vertebral joints. The spinal canal is a hollow tube that houses the spinal nerves. Each nerve exits the spine from both sides of a particular vertebra, branching out to a specific part of the body. Narrowing of the spinal canal exerts more pressure on the nerve, resulting in inflammation of blood vessels and pain along the affected nerve path.
Vertebral facet joints tend to get larger with age. This process is the body’s attempt to decrease the stress per unit area across a degenerated joint. Unfortunately, as the joint enlarges, it exerts more pressure on the nerves branching out from the spine or grow inwards to exert pressure on the nerves emerging from the spinal cord. Standing upright further decreases the space available for the nerve roots and can block blood outflow from around the nerve. Congested blood vessels then irritate the nerve and cause pain. Some people are born with a constitutionally narrow spinal canal; even a small, slipped disc in them can pinch the nerves and cause pain.
When a person rises to a standing position from lying down, there is an additional load on the intervertebral spinal disc. This load causes the spinal disc to bulge while constricting the spinal canal and the foramen. The foramina decrease in size while the nerve roots increase in diameter as you move down the spine. Hence, the lumbar spine in the lower back is most affected.
Causes of Stenosis
The illustrations show a healthy spine and a spine afflicted with stenosis. Pressure exerted on the spinal canal due to an underlying cause such as a compressed spinal nerve is often the cause.
What are the common risk factors for spinal stenosis?
Most people suffering from spinal stenosis are over the age of 50 years. Spinal stenosis in younger people is less likely due to degenerative issues. There are other causes such as trauma, congenital spinal deformities such as scoliosis, and genetic disease. Thorough diagnosis using spinal imaging helps identify underlying causes.
What are the Complications of Spinal Stenosis?
Though rare, untreated severe spinal stenosis may progress and cause permanent:
- Numbness
- Weakness
- Balance problems
- Incontinence of the bladder
- Paralysis in worst-case scenarios
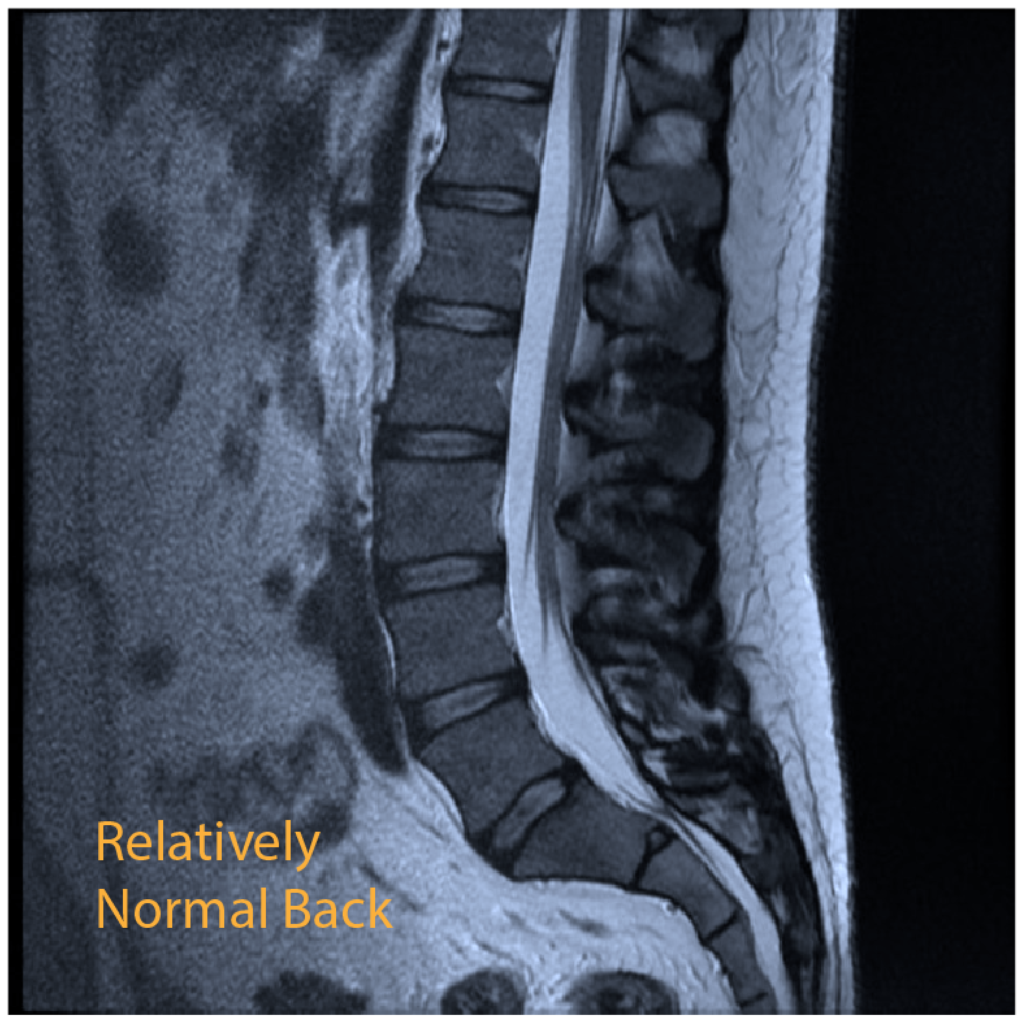
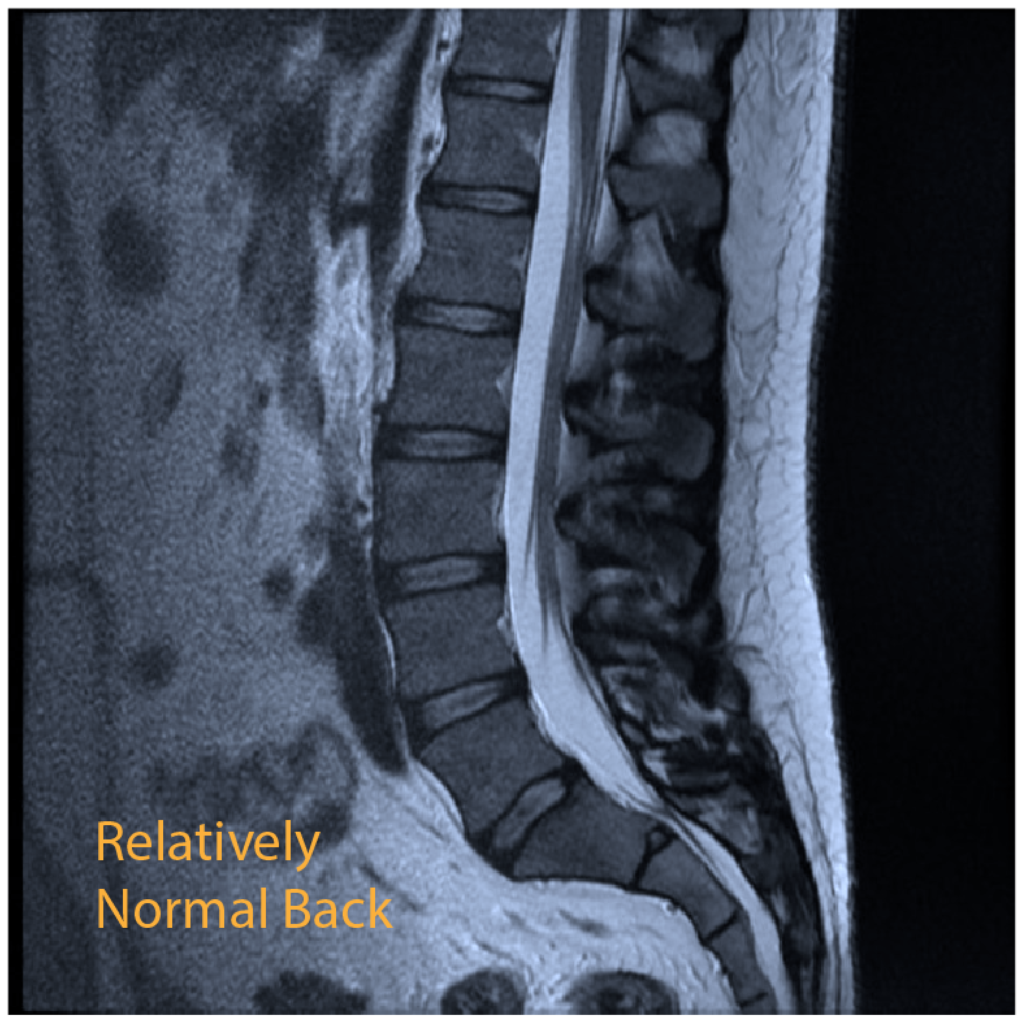
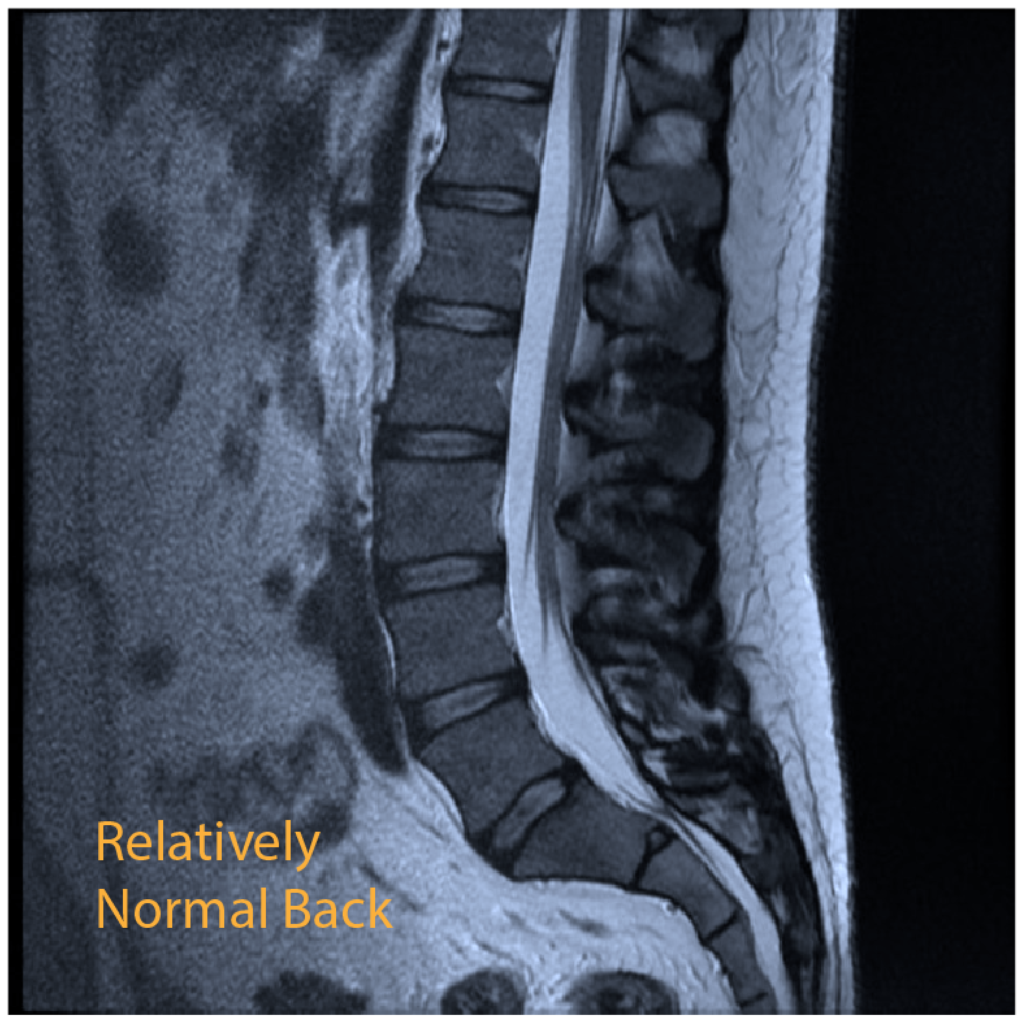
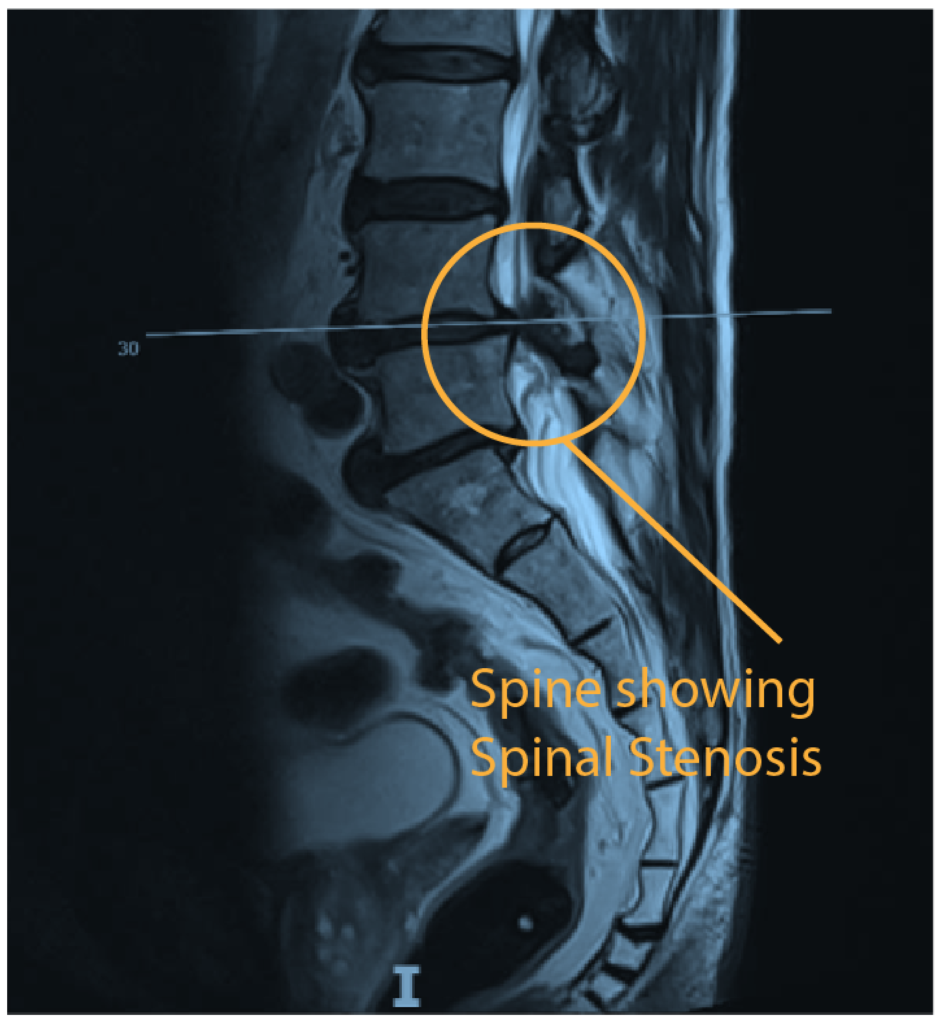
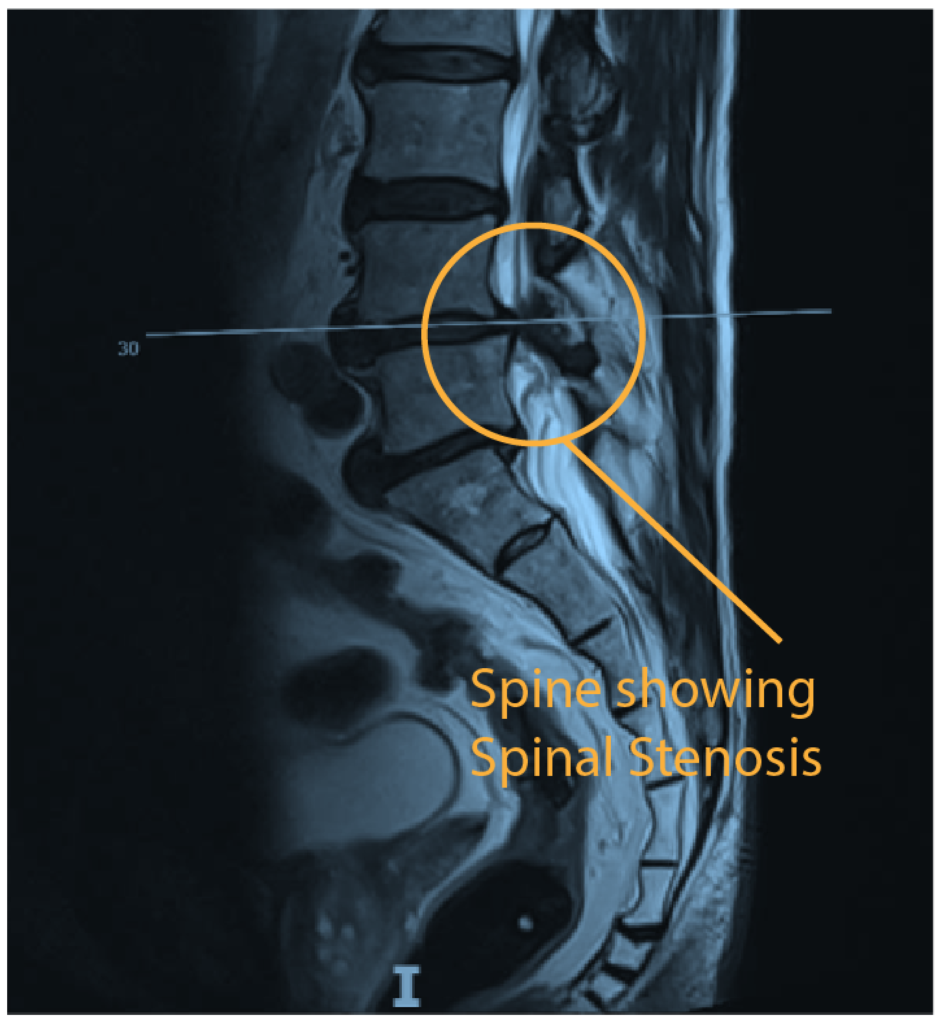
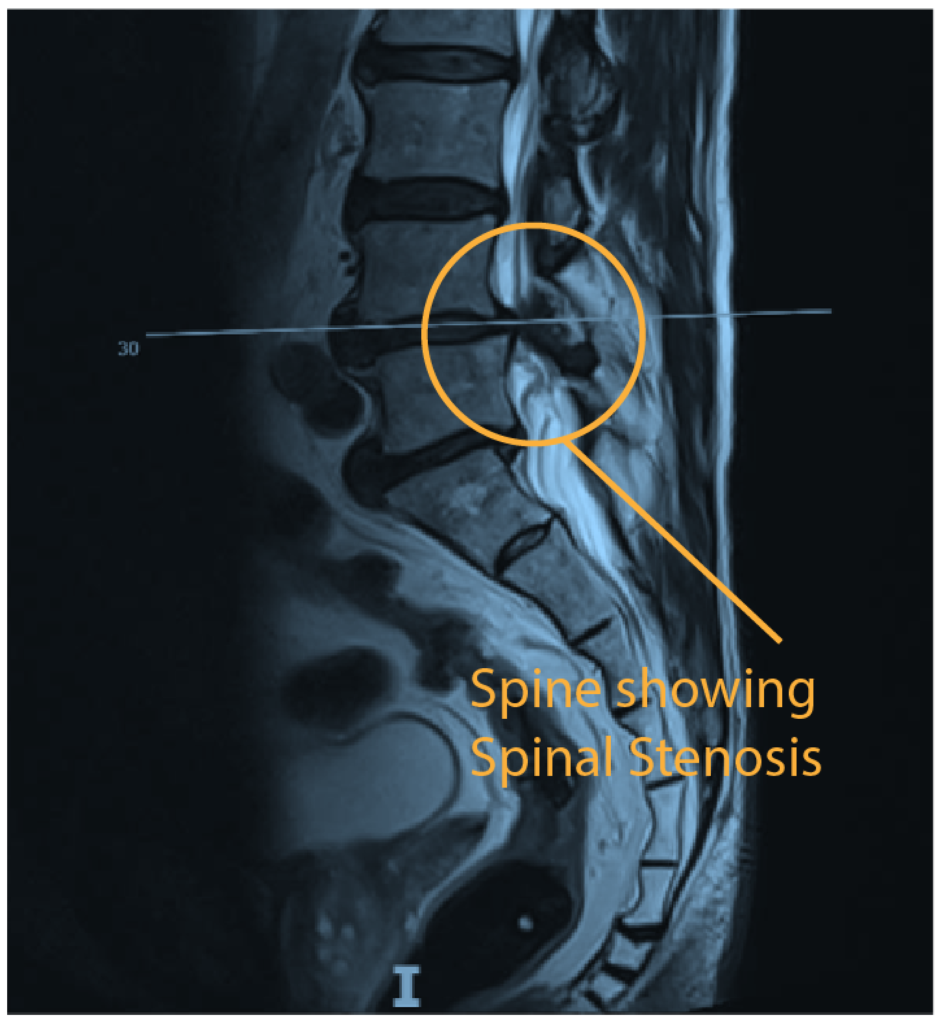
Lumbar Spinal Stenosis seen on a MRI
What are the Treatment Modalities for Spinal Stenosis?
- Ideally, patients start with conventional pain relief treatments, and we only recommend minimally invasive treatments if the pain is not alleviated.
(i) Non-Operative Treatments:
Injections of various kinds around the nerves can help provide temporary pain relief.
Physiotherapy to improve core strength (with massage, ultrasound, TENS, acupuncture, biofeedback, hot or cold packs, traction, or manipulation) can offer symptomatic relief of nerve pain. Unfortunately, such treatments rarely help with claudication or discomfort that worsens on walking.
Osteopathy/Chiropractic care/ Pilates
(ii) Minimally Invasive Treatments- Nerve root block (transforaminal injections):
Improvement of leg pain after injection of anaesthetic is suggestive of lateral recess stenosis.
Epidural steroids can provide reasonable relief for some months.
Sometimes the pain does not improve with non-surgical treatments and worsens while walking. The surgeon will then advise the patient on possible surgery to alleviate the pain and regain regular activity. The most typical reason is stubborn pain, especially in the legs upon walking. A claudication distance of fewer than 300 yards is a standard guide to decide on surgery, but it does depend on the effect on the quality of life.
(iii) Surgery
When both conservative and minimally invasive treatments prove ineffective, they may need surgery. Operative indications include:
- Severe neurological symptoms
- Failed conventional therapy with the inability to walk and affecting your quality of life.
FAQS
What are the diagnostic Investigations carried out to identify spinal stenosis?
The most conclusive investigation is with an MRI scan (without gadolinium). MRI scans currently represents the gold standard in the evaluation of central stenosis. It allows the visualisation of the disc, neural elements, ligamentum flavum and the dura.
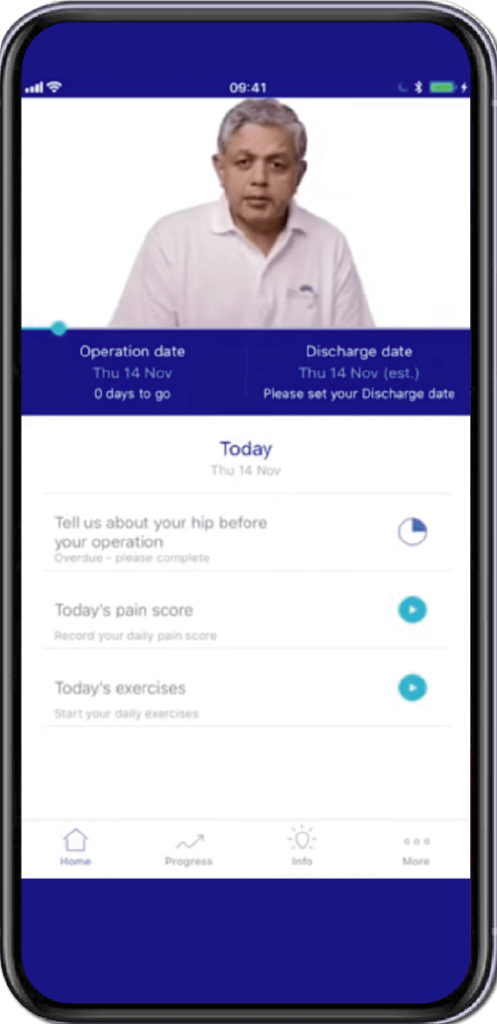
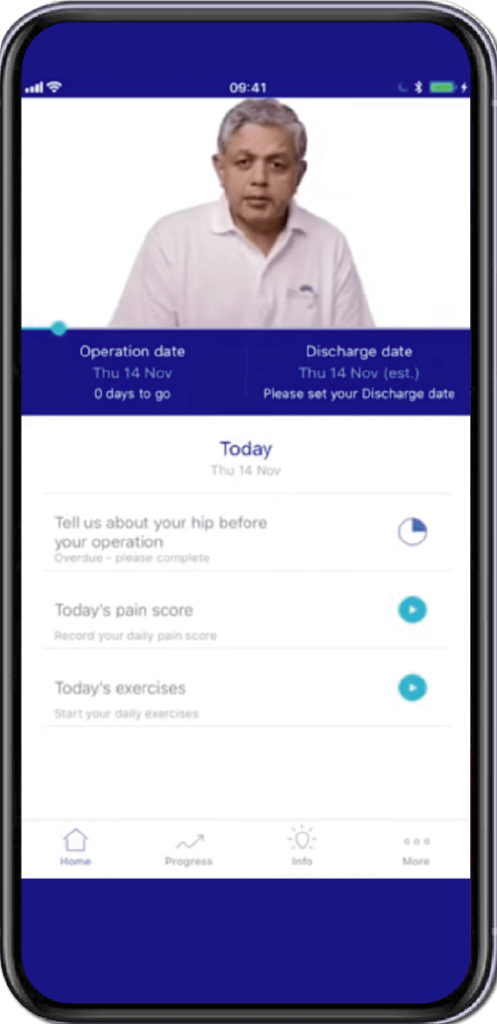
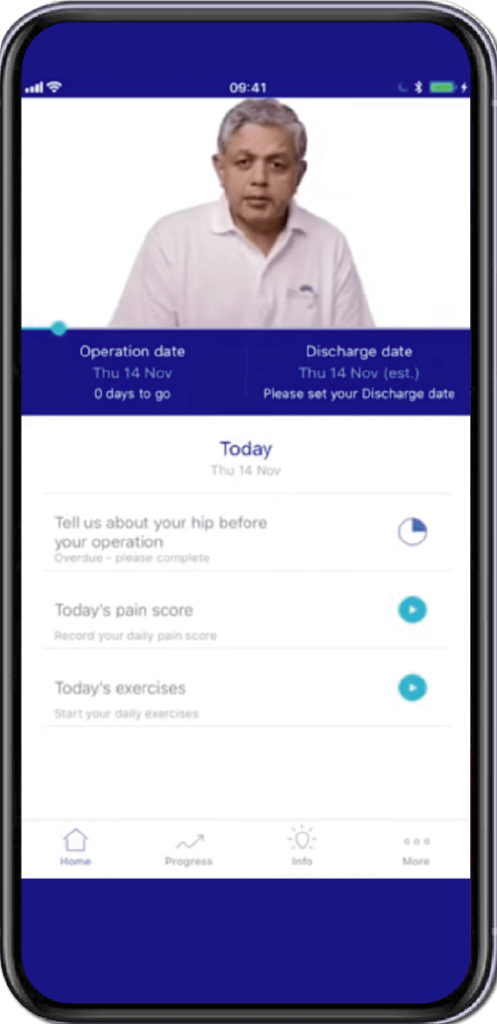
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
