
SCIATICA
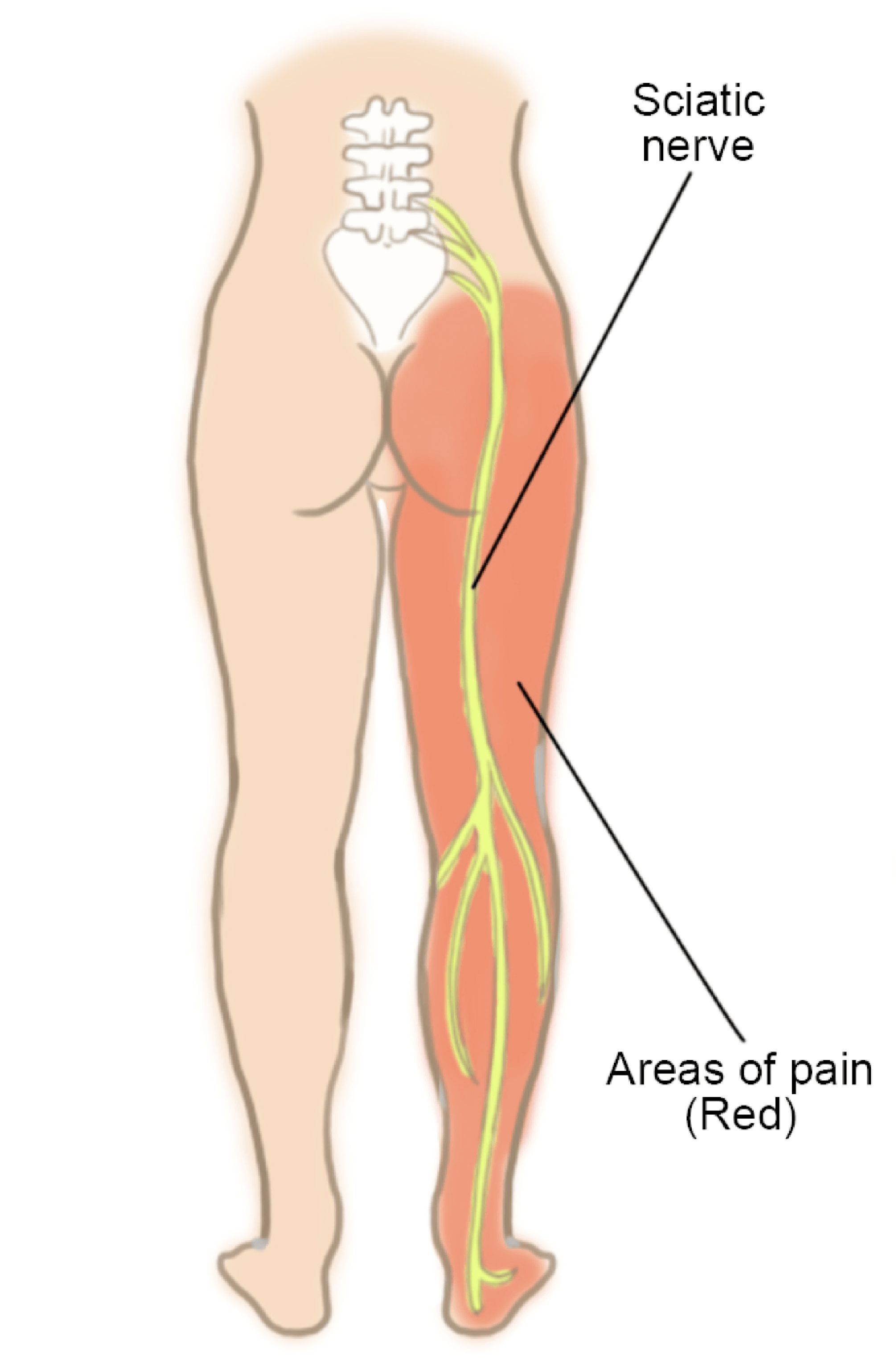
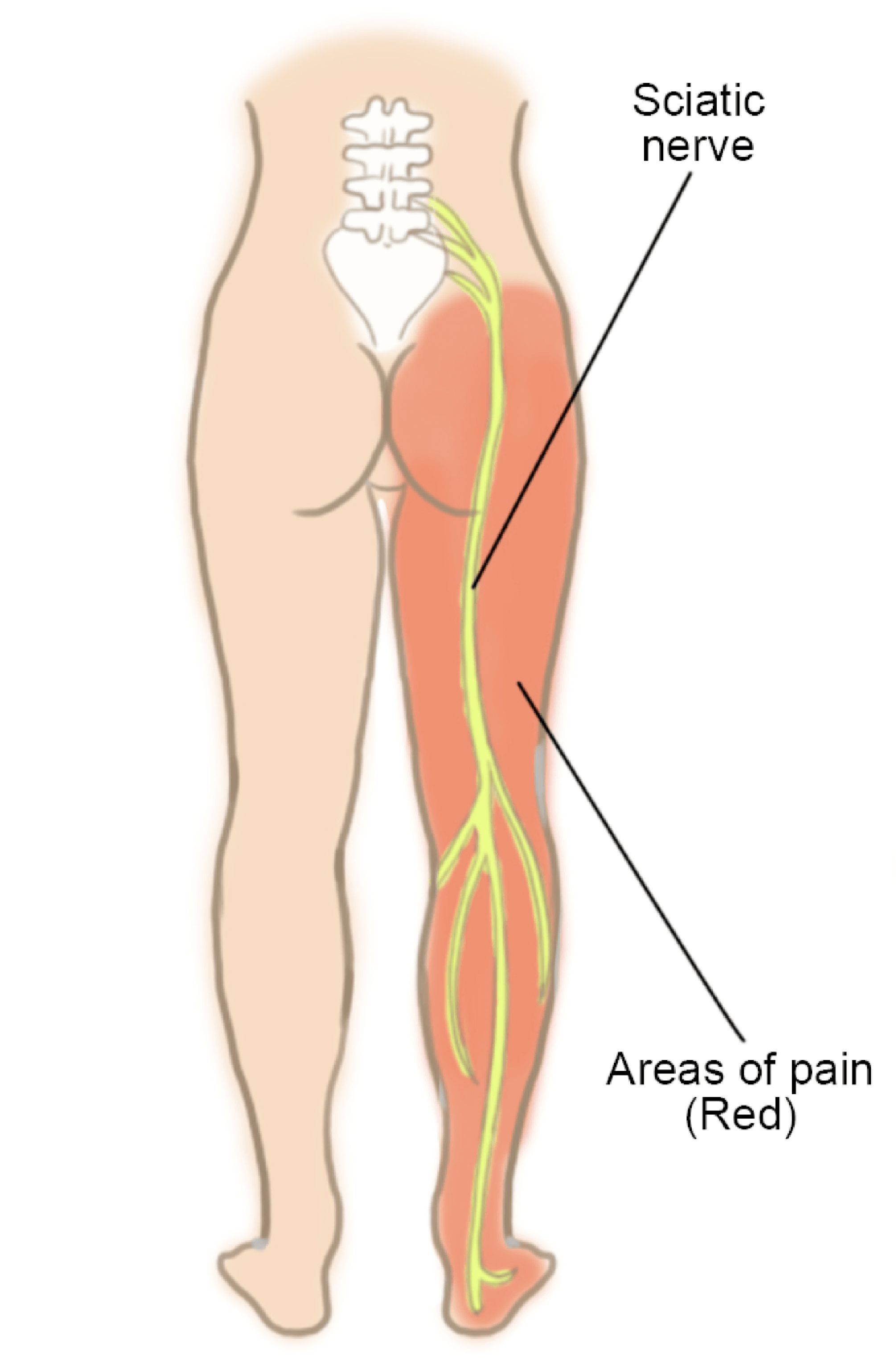
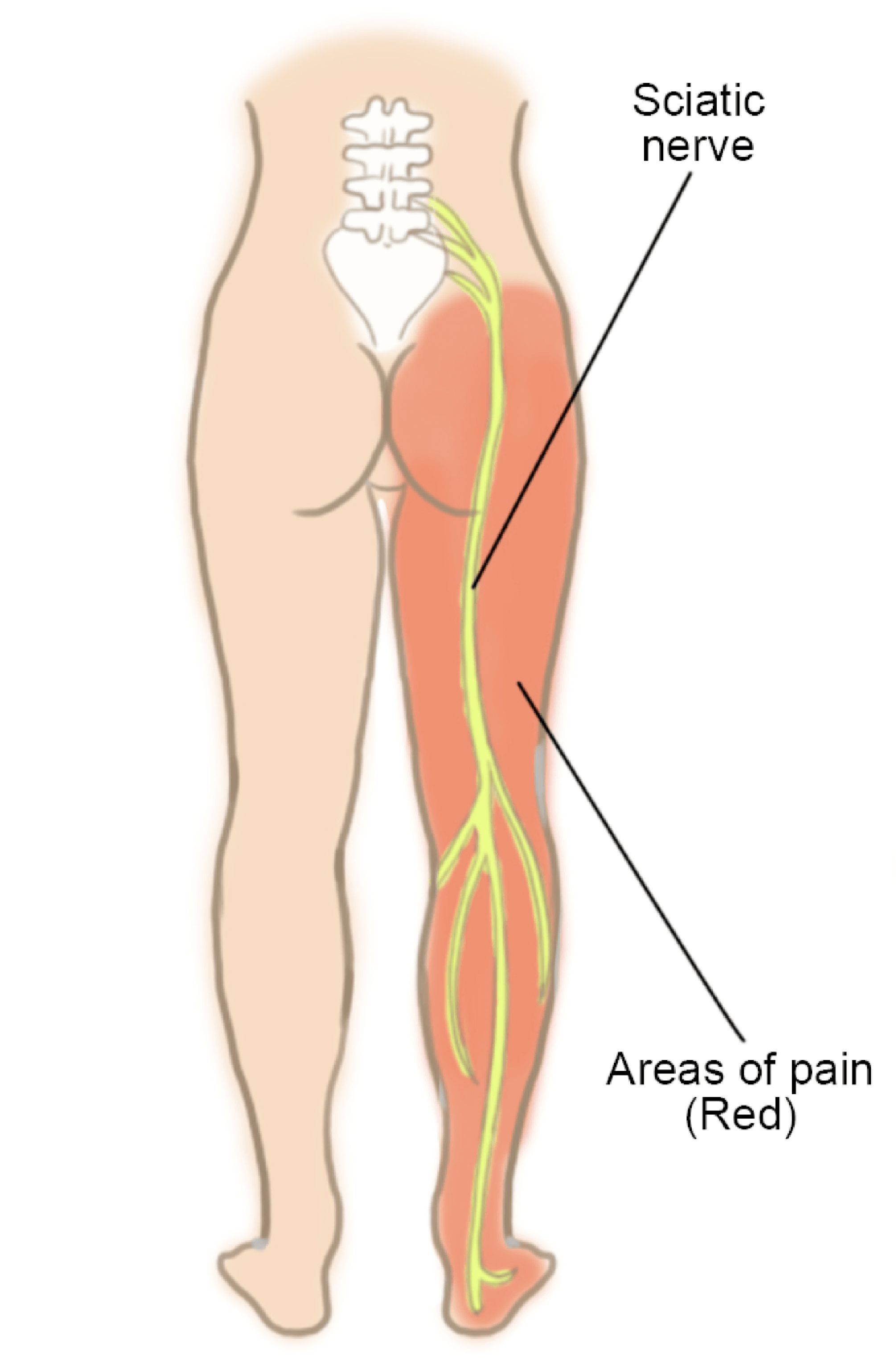
Sciatica is a pain in the lower back that radiates along the sciatic nerve, into the hip, thigh and leg.
What is Sciatica?
The sciatic nerve is the nerve that originates from the lower back and branches out into the leg. When there is pressure on the sciatic nerve, it causes radiating pain along the nerve path especially if the nerve is also inflamed. This pain is known as sciatica. It typically occurs only on one side.
Sciatic neuralgia or sciatic neuropathy is defined as mild to intense pain that radiates from the lower back into either the left or right leg, usually below the knee. This pain often gets worse with movements such as twisting, bending, or coughing. Sciatica affects about 1 in 4 people, most commonly between the ages of 30 and 50.
Though there is a strong genetic influence on sciatica, certain lifestyle factors such as activity, smoking, and occupation can affect one’s propensity for getting sciatica. Usually, people get better with time without any intervention, but sciatica is a very debilitating pain.
Sciatica is not a ‘disease’ as many people believe, but a symptom resulting most commonly from a prolapsed disc or rarely some other pathology along the course of the sciatic nerve outside the spine. Pain could be anywhere along the course of the sciatic nerve that is anywhere from the buttocks all the way down to the ankle.
Patients are worried but once reassured, pain can be managed with pain killers while the condition improves on its own. Despite being extremely painful, 75% of people with sciatica improve substantially within six weeks with conventional non-surgical medical treatment.



Understanding the cause of Sciatic Pain
Sciatica is a pain that often starts in the lower back but radiates along the sciatic nerve into the buttocks or hips and often down the leg into the foot or ankle
What are the Typical Symptoms of Sciatica?
You may typically notice the following symptoms:
- Pain- constant burning sensation or a shooting pain radiating from the lower back or buttock and all the way down the front or back of the thigh and leg and/or feet.
- Numbness- Often accompanied by numbness in the back of the leg and at times, tingling and weakness too.
- One-sided symptoms- Sciatica typically affects one leg resulting in a feeling of heaviness in the affected leg. Both legs are rarely affected together.
- Posture-induced symptoms- which get worse while sitting, trying to stand up, bending the spine forward, twisting the spine, lying down, and/or while coughing. The symptoms may be relieved by walking or applying a cold pack over the lower back.
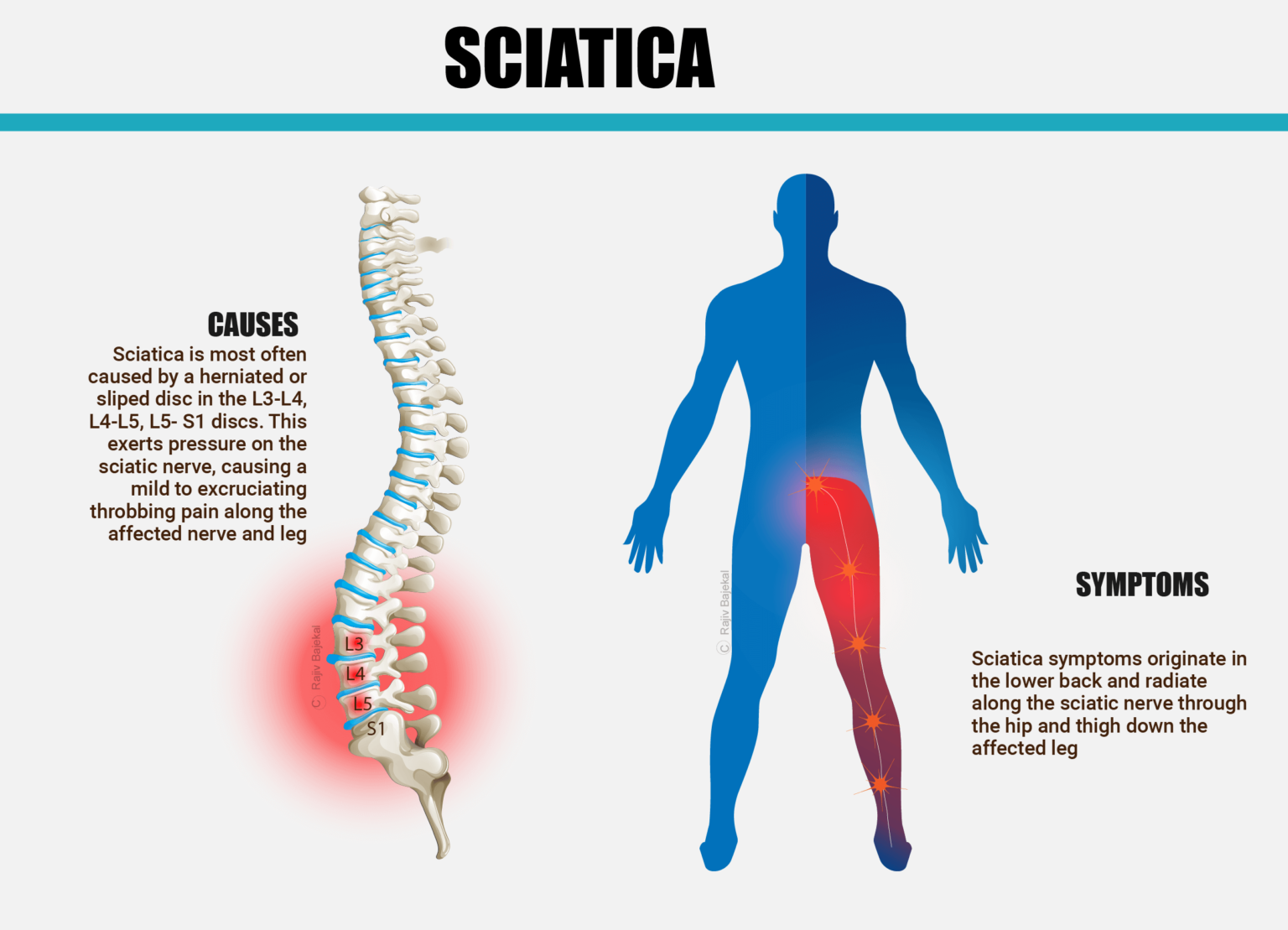
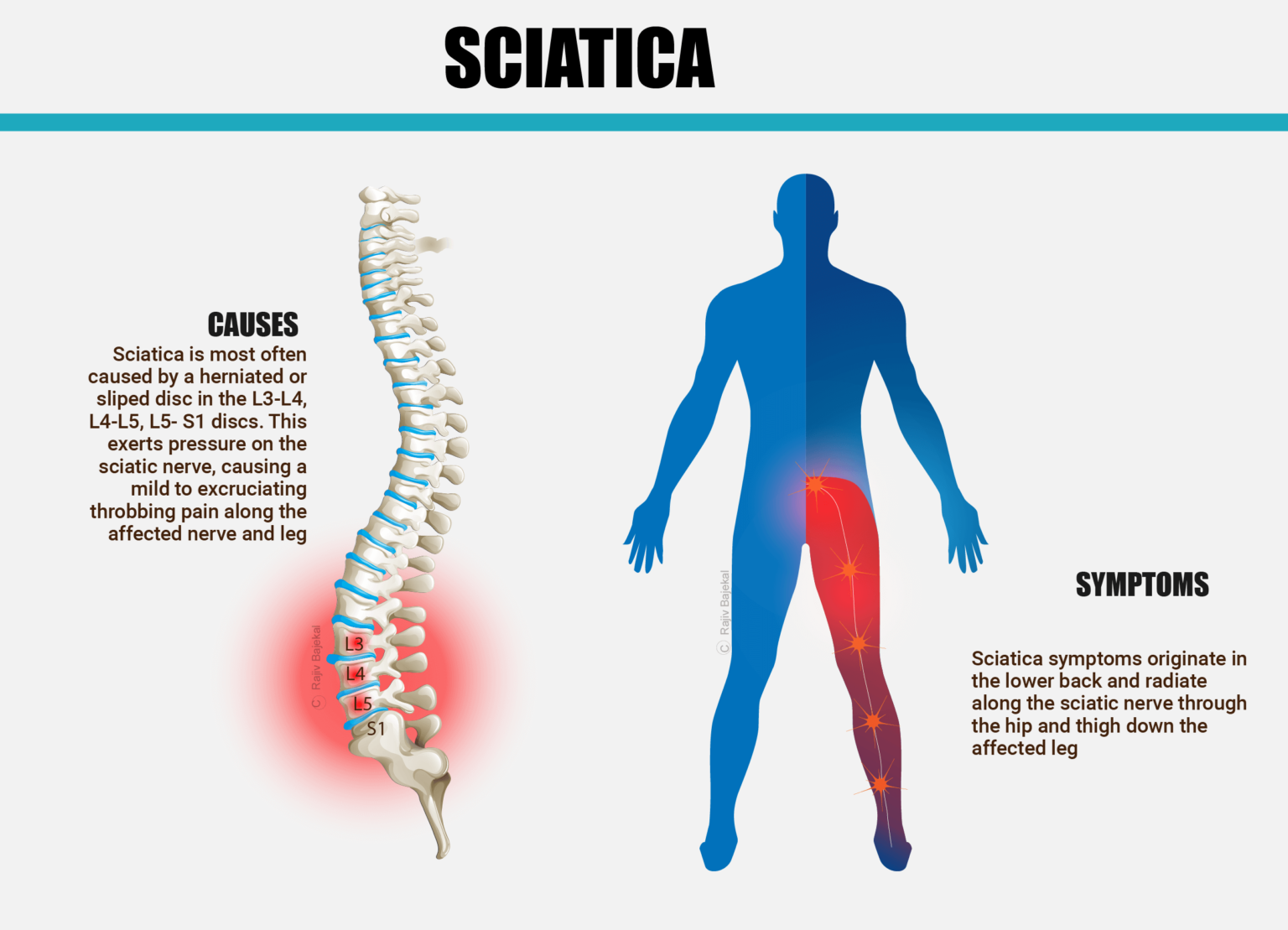
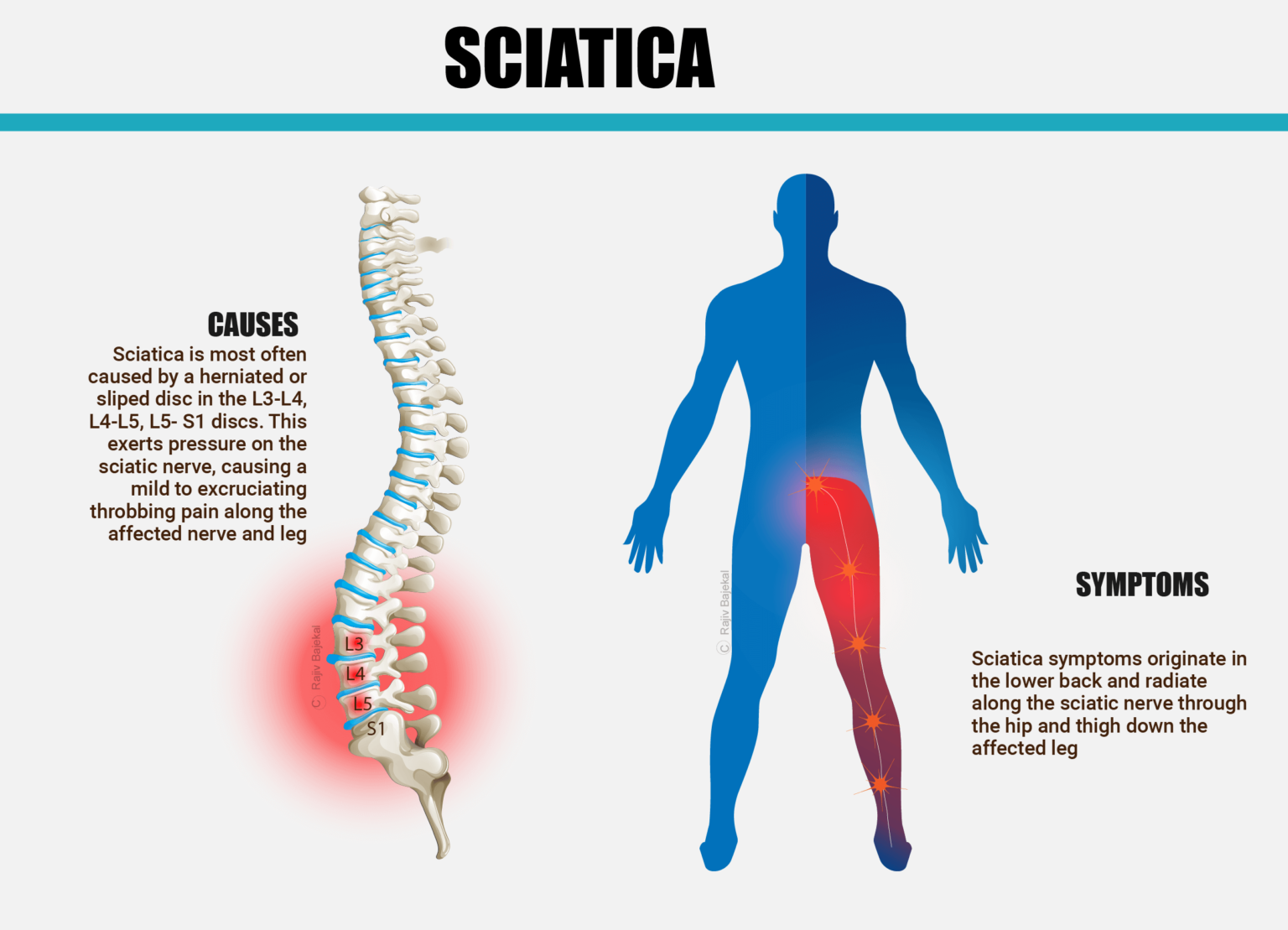
What are the Common Causes of Sciatica?
Poor core strength, being overweight and lower spinal disc water content can contribute to conditions leading to sciatica. The water content of the intervertebral discs naturally reduces with age, making it more prone to injury and herniation. Unhealthy lifestyle choices can worsen this.
This pain is typically caused either by a herniated disc or slipped disc (url/link-page) in the lower spine or sometimes by lumbar spinal stenosis (url/link-page) brought about by narrowing of the spinal canal most commonly in the lowest three discs. When the nucleus (gel-like inside) of the disc protrudes into or through the annulus (disc’s outer lining), the resulting herniated disc presses directly on nerve roots that form the sciatic nerve, leading to sciatica. Sometimes, the nerve can also get inflamed and irritated by chemicals from the disc’s nucleus and cause sciatica.
SOME STATISTICS ABOUT SCIATICA THAT YOU MAY FIND HELPFUL
2% of the population experiences a herniated disc.
Only 10-25% have symptoms lasting more than six weeks.
80-90% of patients suffering with sciatica get better with time, without surgery.
What are the factors which increase my risk of getting sciatica?
Factors contributing to sciatica include:
- Genetic factors – Dietary factors that cause atherosclerosis and narrowing of the blood supply to the vertebrae and therefore nutrition of the disc
- Improper lifting
- Poor posture
- Smoking
- Excess weight -that places added stress on the discs(in the lower back)
- Sudden pressure (which may be slight)
- Repetitive impact activities.
- Rarely accidents
All these factors result in ‘wear and tear’ of the disc and make them more susceptible to damage.
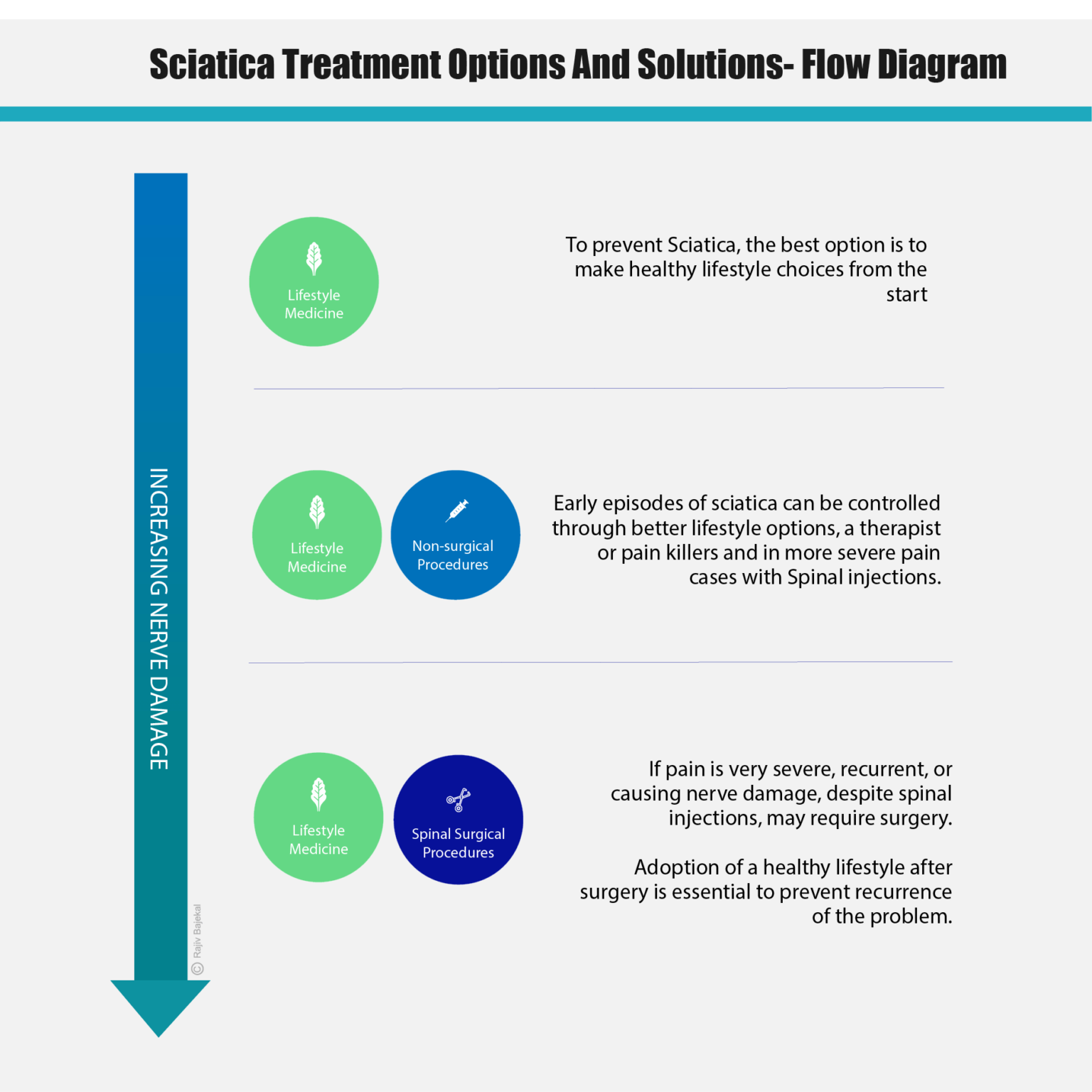
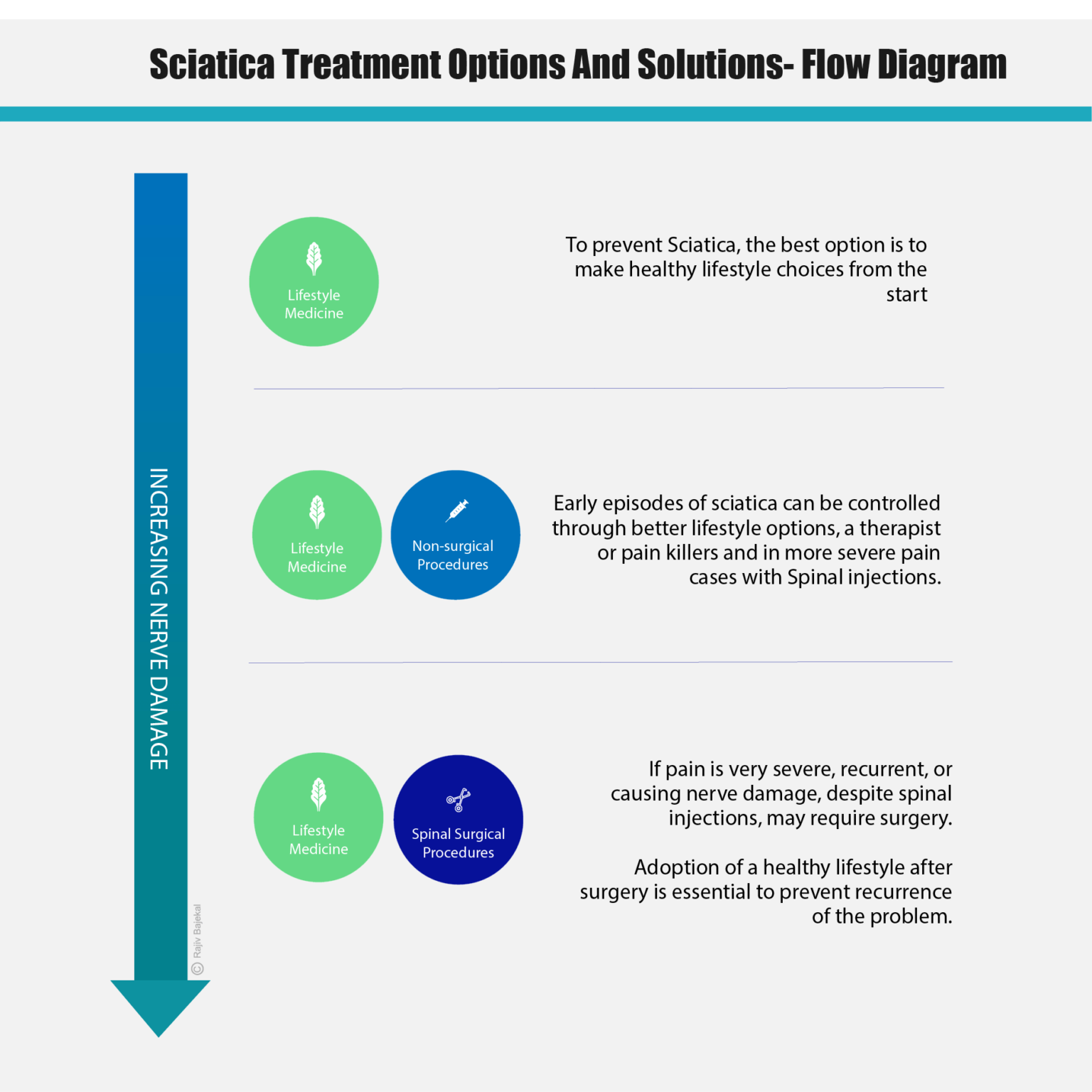
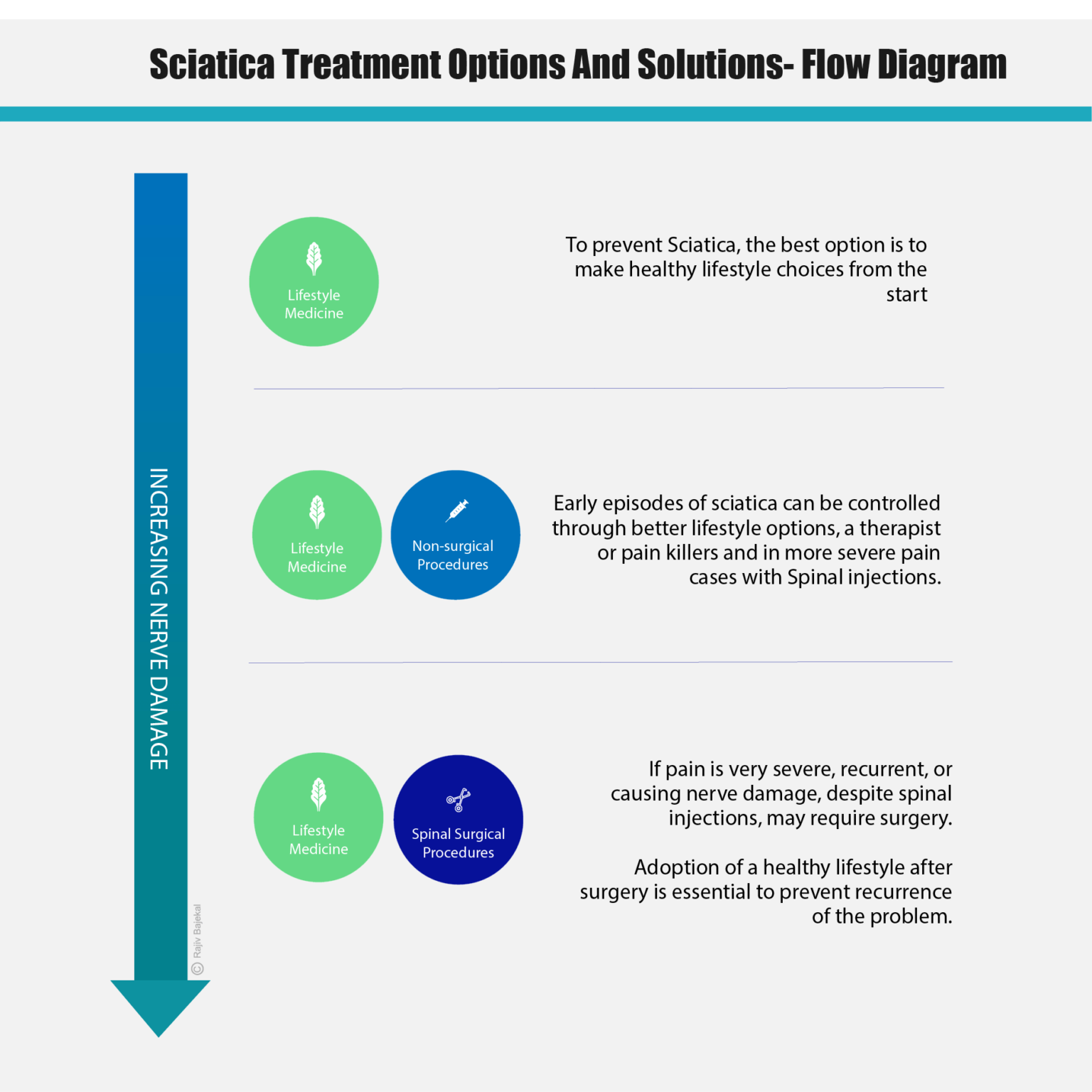
How is Sciatica treated?
Sciatic pain can be of varying intensity, in the early stage it can be managed with the use of over the counter pain killers along with exercise and lifestyle changes to find relief. Often the pain settles in a few days to weeks.
Lifestyle changes include a better diet regular physical movement and exercise, yoga, quitting smoking and adopting better postures for sitting, standing, sleeping, and lifting.
But with time, if one does nothing, continuous additional pressure can start damaging the sciatic nerve. If the pain does not respond to regular pain killers or starts interfering with your day to day life, more specific pain management, alternative medical options or non-surgical interventions or even surgery may be needed.
What dietary changes may help with managing my sciatica?
Adopting a plant predominant diet rich in fruit, vegetables, whole grains, beans and small amounts of nuts and seeds rather than ultra-processed foods, sugar sweetened beverages and a diet rich in meat, eggs and dairy will help as will efforts to improve the quality of sleep, exercise, and relaxation. (lifestyle medicine – url/link-page) (hyperlink to Lifestyle medicine leaflet ).



Mackenzie Exercises and Physiotherapy
These are simple and often highly effective exercises that address the core issue in our day-to-day life, based on Dr Robin Mackenzie’s principles. The McKenzie Exercise Method is a therapeutic approach that requires you to move through a series of exercises and test movements to gauge your pain response. Physiotherapists use the information to develop an exercise protocol designed to relieve the pain.
Physiotherapy, yoga, quitting smoking and developing a better posture also have a role in helping to manage the pain.
When should I seek medical help?
It is quite common to seek help from allied health professionals such as Osteopaths or Chiropractor. Often their understanding of this symptom and the reason it is so painful, is excellent. With their ability to do hands on work on your back and their ability to ease muscle spasms, they can help during the acute phase of sciatica. If you are medically insured, please check whether you could be covered for treatment with a therapist. I often refer people to an allied health professional if appropriate.



What can be done to manage my sciatica?
Medical
This aims to manage pain without long-term use of medications. Firstly, you may need at least a few days of bed rest (up to 2 days while the inflammation settles.) Non-steroidal anti-inflammatory medication (NSAIDs) such as naproxen, ibuprofen, aspirin, or muscle relaxants are also helpful. More severe pain may need more potent pain killers such as codeine, dihydrocodeine or co-codamol. Cold compresses on painful muscles also help.
For more advice on pain management, you should speak to your general practitioner. If pain management becomes difficult, your doctor may need to refer you to a specialist like myself for consideration of investigations and further management.
Acupuncture
Some people find it to be of great help to reduce sciatic pain.
Posture, Rest and Exercises for Sciatica
You should continue to be as active as possible as moving helps to reduce inflammation. You should find comfortable positions to sit or lie down, which can reduce the intradiscal pressure and give you some relief from your sciatica symptoms.
Focus on Strengthening Core Muscles
When should I go to the doctor? What should I expect?
If the pain is interfering with your work and daily chores, it might be a good idea to see the doctor. More worrying symptoms such as severe bilateral leg pain, numbness in the bottom and private areas, incontinence, or inability to feel the bladder filling up are indicative of the more serious cauda equina syndrome. You must attend Accident and Emergency department of your nearest hospital if in doubt, or if you are concerned.
You should provide details to the doctor, such as when the pain started, where it travels and precisely how it feels when aggravated. A physical examination may help pinpoint the irritated nerve root. Your doctor may ask you to squat and rise, walk on the heels and toes, or perform a straight leg raising test or other tests. Most cases of sciatica affect L5 or S1 nerve roots. An MRI (magnetic resonance imaging) scan may be needed to confirm which nerve roots are affected.
What happens in the MRI scanner (magnetic resonance imaging)?
The MRI scan is generally able to detect which disc is exerting pressure on the sciatic nerve. MRIs are a modern diagnostic imaging technique that produces cross-sectional images of the body. Unlike CT scans, MRI works without radiation. The MRI tool uses magnetic fields and a sophisticated computer to take high-resolution pictures of bones and soft tissues.
You must inform us if you have implants, metal clips, pacemakers, or other metal objects in your body before undergoing an MRI scan. It is also best avoided in the first trimester of pregnancy unless absolutely necessary.
An MRI is a very safe investigation, but it can provoke claustrophobia and is often noisy. It is always best to close your eyes before your table is slid into the machine and open your eyes after the procedure if you are prone to claustrophobia. Sometimes a mild sedative taken before you undergo a scan makes it possible even for people who are claustrophobic to undergo an MRI.
If you are very claustrophobic, do let me know and I can arrange an alternative test or a wide open scan.
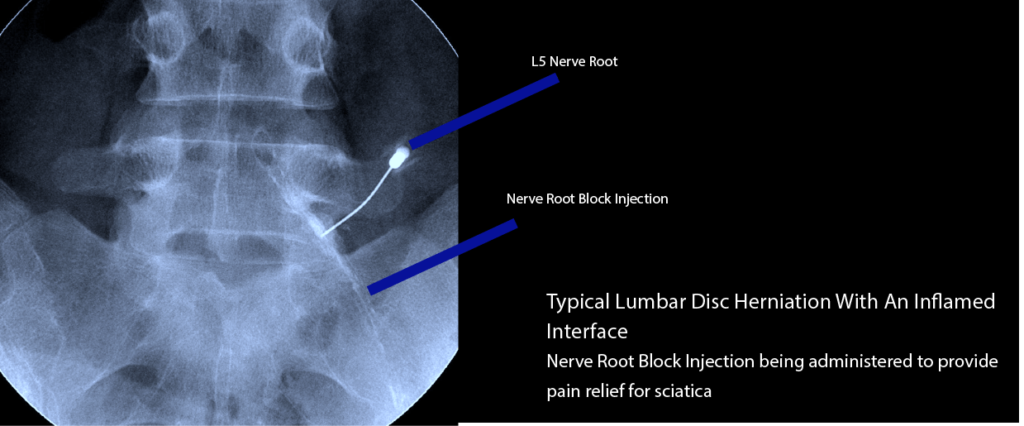
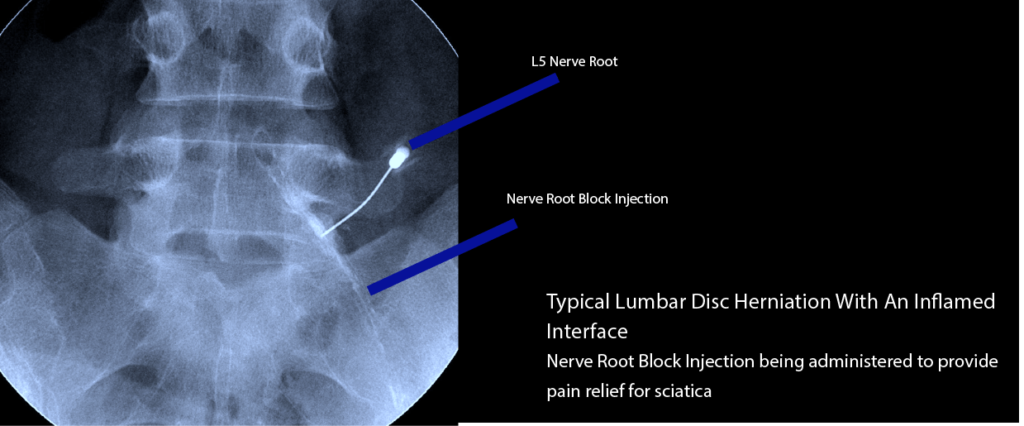
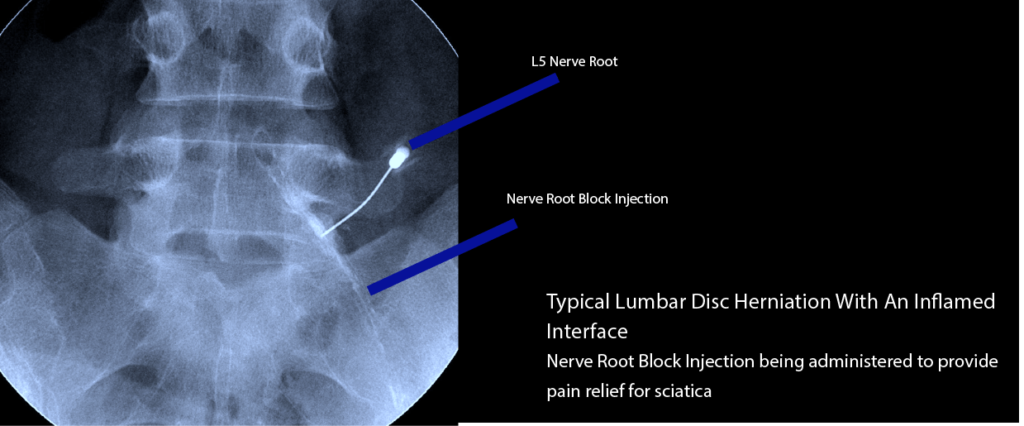
An MRI scan allows us to be certain about which level of the spine is affected and more specifically, which nerve root is inflamed. This helps us treat the condition by a targeted injection.
Non-surgical Treatment
Injection treatment
Most times, sciatic pain will get better within a few weeks and in fact the natural history is that 75% of patients get better within 6 weeks. When pain is uncontrollable with medication, the I may discuss intervention such as a nerve root block (transforaminal epidural) or a caudal epidural injection, which can quickly provide dramatic relief. Often injections settle the pain within 2-3 days, allowing patients to return to work. Pain relief may be long lasting, not because the injection acts ‘forever’ but because the natural history may improve the condition by itself. These are not numbing injections and do not increase the possibility of causing further damage by reducing awareness.
Injections tend to improve pain by reducing the inflammation at the interface between the herniated disc and the nerve root. Chemical mediators from the nucleus, which act as nerve irritants, are counteracted by the washing out effect of the injection and possibly the steroid.
Surgical Treatment of Sciatica
If non-surgical methods are unsuccessful in helping with sciatica or the slipped disc is causing damage to the nerves and weakness in the leg, there is a role for surgery, and this is discussed under discectomy (url/link-page).
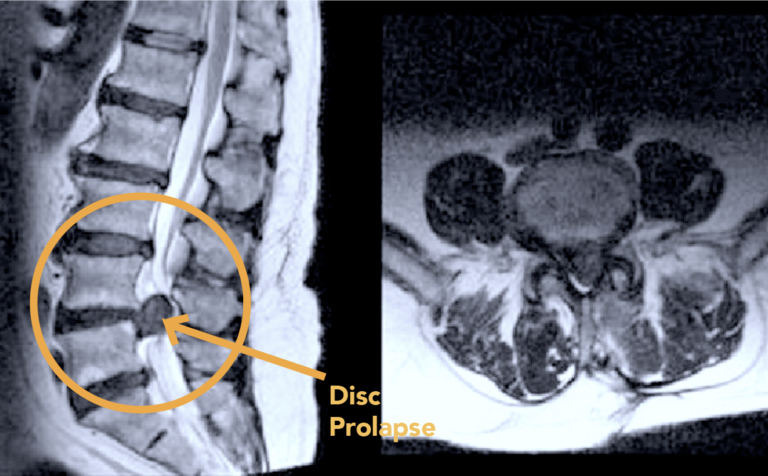
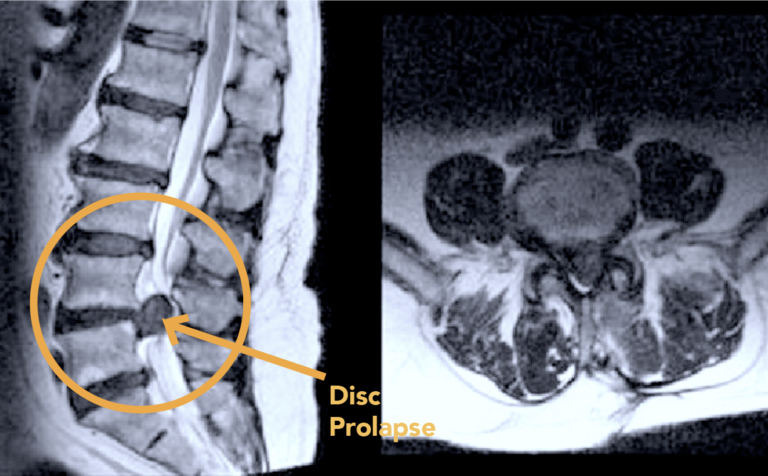
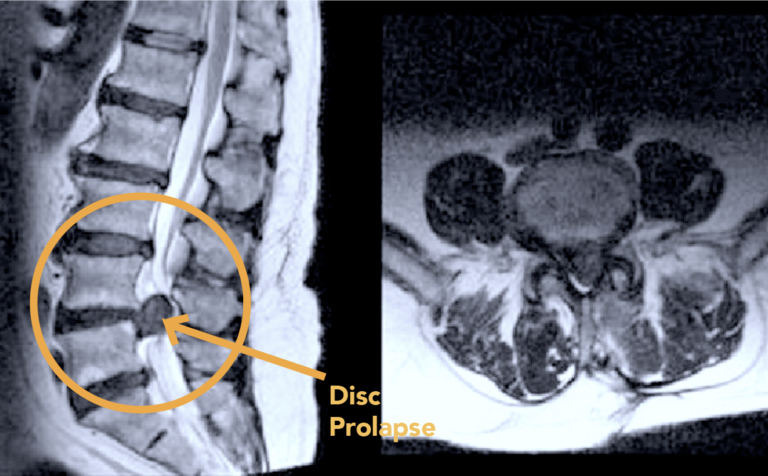
MRI appearance of a Disc Prolapse
The Disc Prolapse is clearly seen in the adjoining MRI.
FAQs
When should I see you? I am in terrible pain will you be treating me at the consultation?
No, a consultation is just that and although we will endeavour to expedite all tests and further treatment I will not be able to ‘cure’ you on the first consultation. Pain medication is best prescribed by your family doctor as they have your complete medical history and know what suits you.
Do I need a referral letter from my GP?
Ideally yes, this letter will be full of valuable information in the form of your medical history which will help enable me to diagnose your condition better. We like to keep the referral letter on file. Please bring this letter along with you.
I already have MRI scans. Should I bring these with me?
Yes, to all consultations as these are an especially important diagnostic tool and I will need to refer to these often. The report is not sufficient, I will need to see the pictures to make a diagnosis. If you do not have the images, speak to Dawn Flatt our practice manager on 0208 4497624 and she may be able to help in getting hold of the images.
What can I expect at my consultation?
If the pain is interfering with your work and daily chores, it might be a good idea to see me. More worrying symptoms such as severe bilateral leg pain, numbness in the bottom and private areas, incontinence, or inability to feel the bladder filling up are indicative of the more serious cauda equina syndrome and mandate attendance to accident and emergency departments.
You should provide details to me, such as when the pain started, where it travels and precisely how it feels when aggravated. A physical examination may help pinpoint the irritated nerve root. I may ask you to squat and rise, walk on the heels and toes or perform a straight leg raising test or other tests. Most cases of sciatica affect L5 or S1 nerve roots. X-rays and other specialised imaging tools such as MRI (magnetic resonance imaging) can confirm my diagnosis of which nerve roots are affected.



Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
