
Vertebral Compression Fractures (Osteoporotic)
As Osteoporosis advances, it can lead to painful fractures in the body. Reducing bone density with age is a major contributor. In the spine, these are known as vertebral compression fractures.
What are Vertebral Compression Fractures?
As Osteoporosis advances, it can lead to painful fractures in the body. Reducing bone density with age is a major contributor. In the spine, these are known as vertebral compression fractures. When a vertebra in the spine collapses it often causes pain, deformity of the spine and loss of height. These fractures most commonly occur in the thoracic and lumbar regions in the spine. The leading cause of VCFs is low bone density caused by advanced stages of osteoporosis. More than 3 million women in the U.K. have osteoporosis.
If Osteoporosis is neglected, it can lead to complications as it advances. Moderate Osteoporosis usually requires force and trauma such as falling or lifting a heavy object before it results in a vertebral compression fracture. However, with advanced cases of osteoporosis, a VCF can occur even while performing simple daily activities, like stepping out of the shower, sneezing forcefully, or trying to lift a light object.
Non-osteoporotic VCFs can occur, but are usually due to accidents, trauma injury to the vertebrae and even cancer.
VERTEBRAL COMPRESSION FRACTURES






How common are Vertebral Compression Fractures?
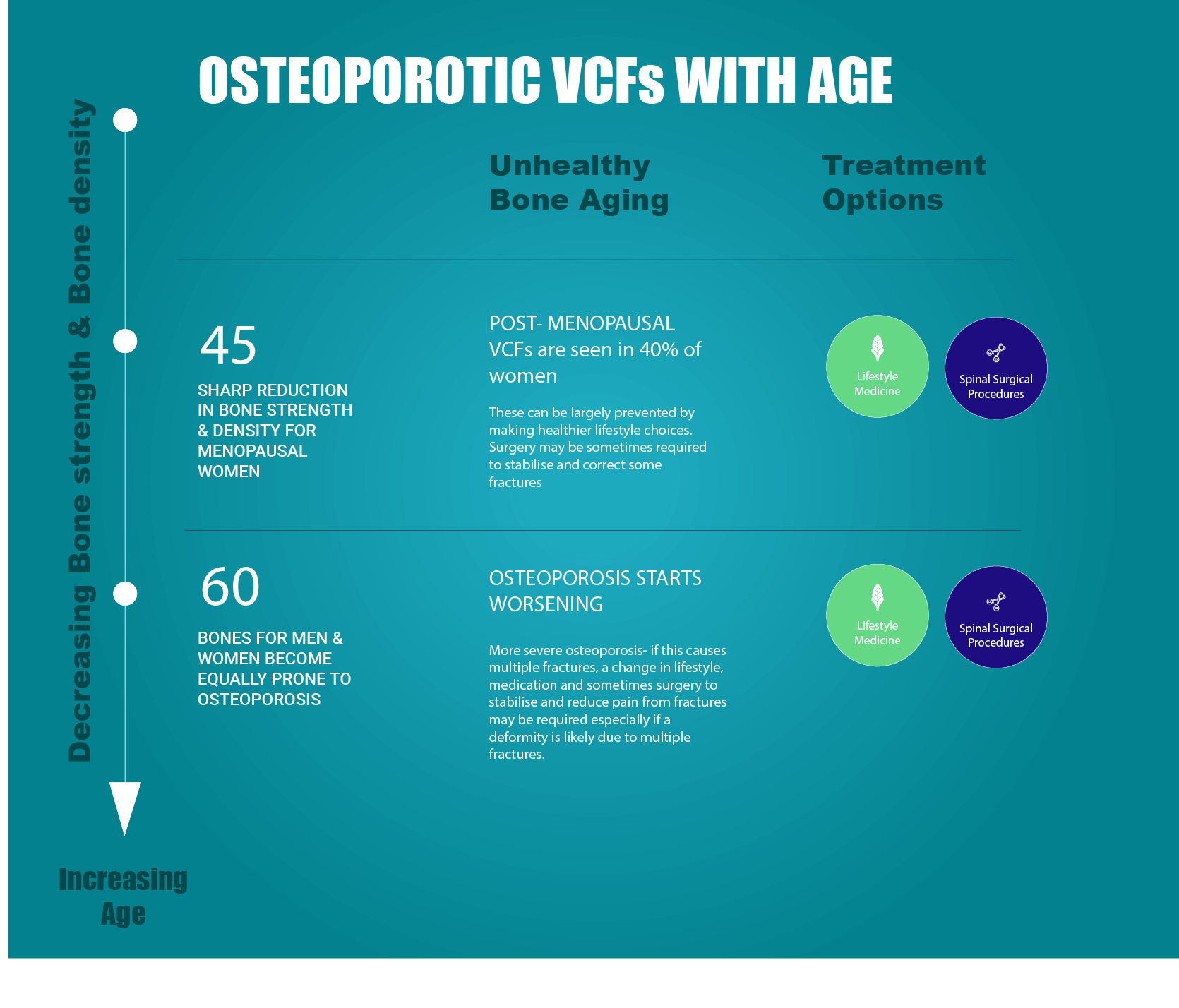
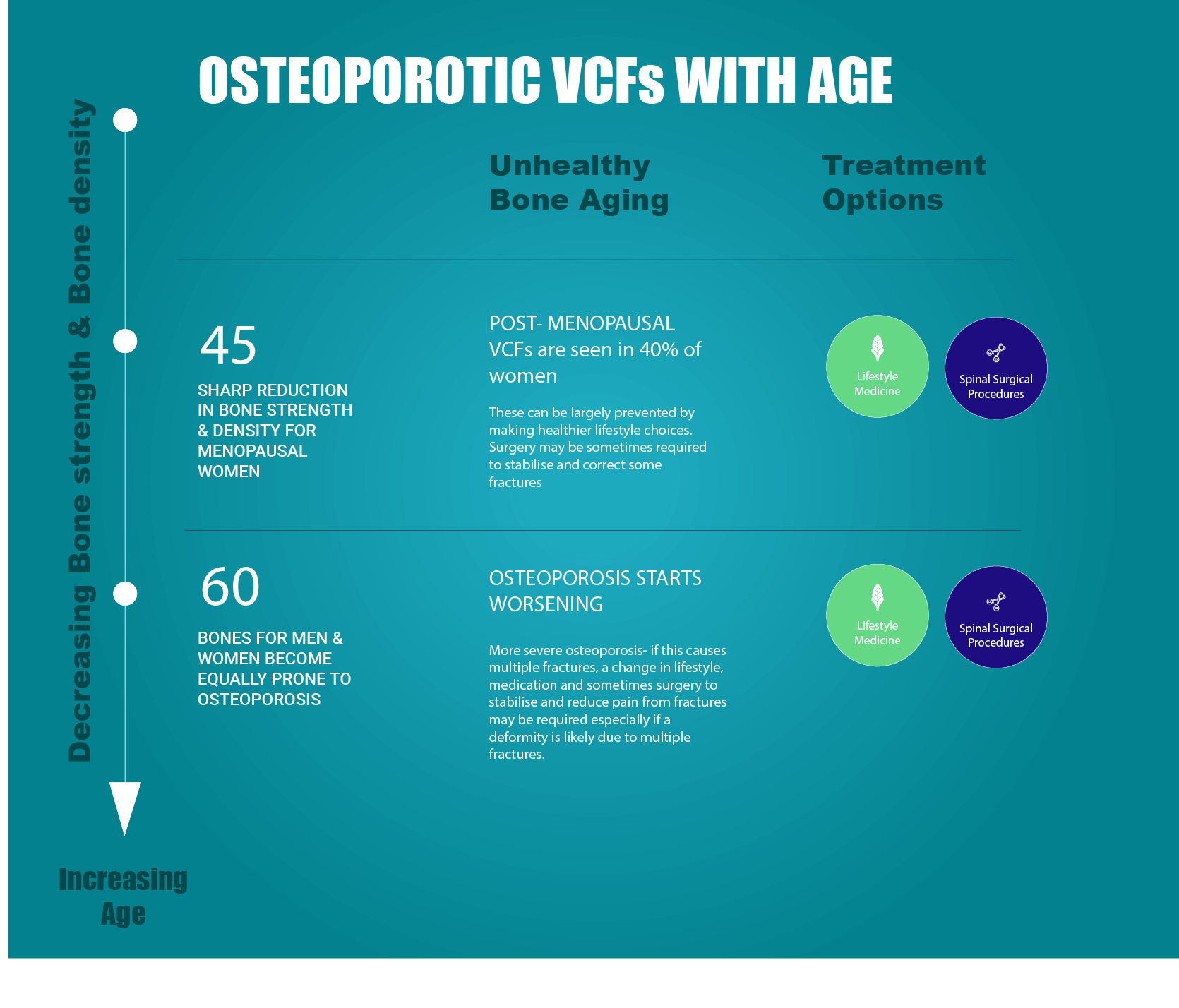
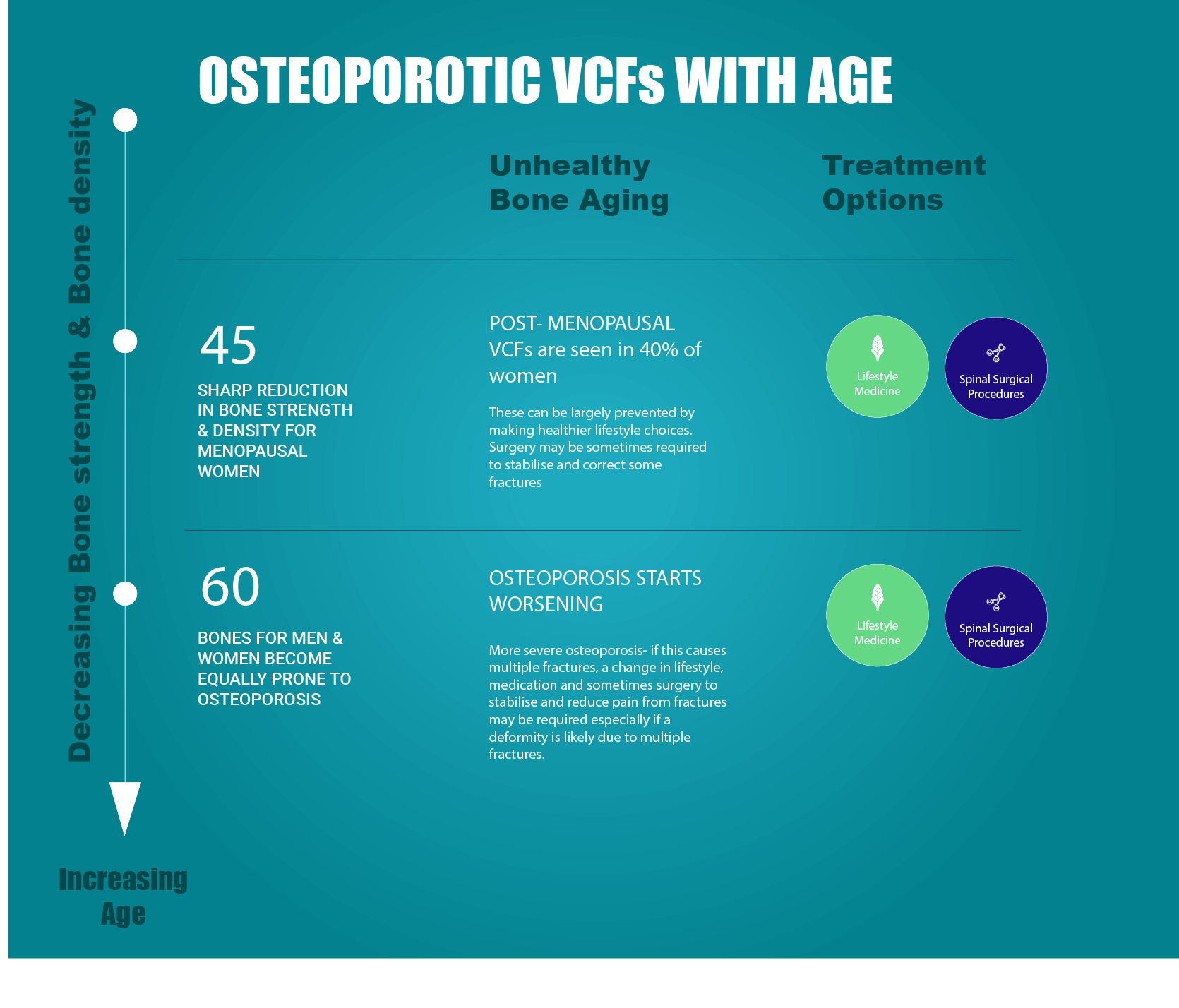
VCFs are quite common fractures in patients with osteoporosis. According to the NHS, approximately 3 million people in the UK are believed to suffer from osteoporosis. Statistics indicate that there are over 230,000 fragility fractures in the UK each year as a result, many of these being VCFs. Patients who have had one osteoporotic VCF are sadly at five times the risk of sustaining a second VCF. Sometimes, a VCF can be present with either minor symptoms or no symptoms, but the risk still exists for additional VCFs to occur. It is estimated that 25% of all postmenopausal women will suffer osteoporotic VCFs. The occurrence of VCFs steadily increases with advancing osteoporosis. It is estimated that 40% of women aged 80 and older are affected. It is important to note that though VCFs are more common in women, they are also a major health concern for older men after 60 men as they may also suffer from osteoporosis.
With progressing age, osteoporosis can result in painful compression fractures in the spine resulting in stooped posture and height loss, and sudden back pain. It is best to improve one’s lifestyle to prevent osteoporosis or at least delay its onset.
What are the typical symptoms of VCF?
Clinical symptoms of VCFs can include any or a combination of the following:
- Sudden excruciating back pain
- Increasing pain intensity if standing or while walking
- Decreased pain intensity while lying on the back
- Reduced spinal mobility
- Decrease in height
- Eventual deformity and disability
How Does One Reach A Diagnosis Of VCF?
Ideally, it is best that one goes to an orthopaedic to have their spine examined before embarking on any diagnosis. They will offer the best way forward, depending up on the condition of the patient.
I may recommend certain diagnostic tests to confirm the presence of a vertebral compression fracture. I would do this after conducting a physical examination and taking a detailed clinical history, including risk factors and any other reports if available. It is important to note that osteoporotic VCFs often present no symptoms and can occur without warning. I may suggest x-rays, computed tomography (C.T.) or a magnetic resonance imaging (MRI) to confirm the diagnosis of a VCF. This would help to predict the prognosis and determine the best treatment option for you going forward.
Often an MRI scan is the best way to reach a diagnosis because it tells us which of the fractures are fresh and which ones are old and healed. Bone marrow oedema is best seen on a STIR sequence. It also gives us an idea about whether the fracture is treatable by surgery (see Balloon kyphoplasty).
What Treatments Are Used To Treat Vcfs?
(a) Pain Relief and Non Surgical Treatments
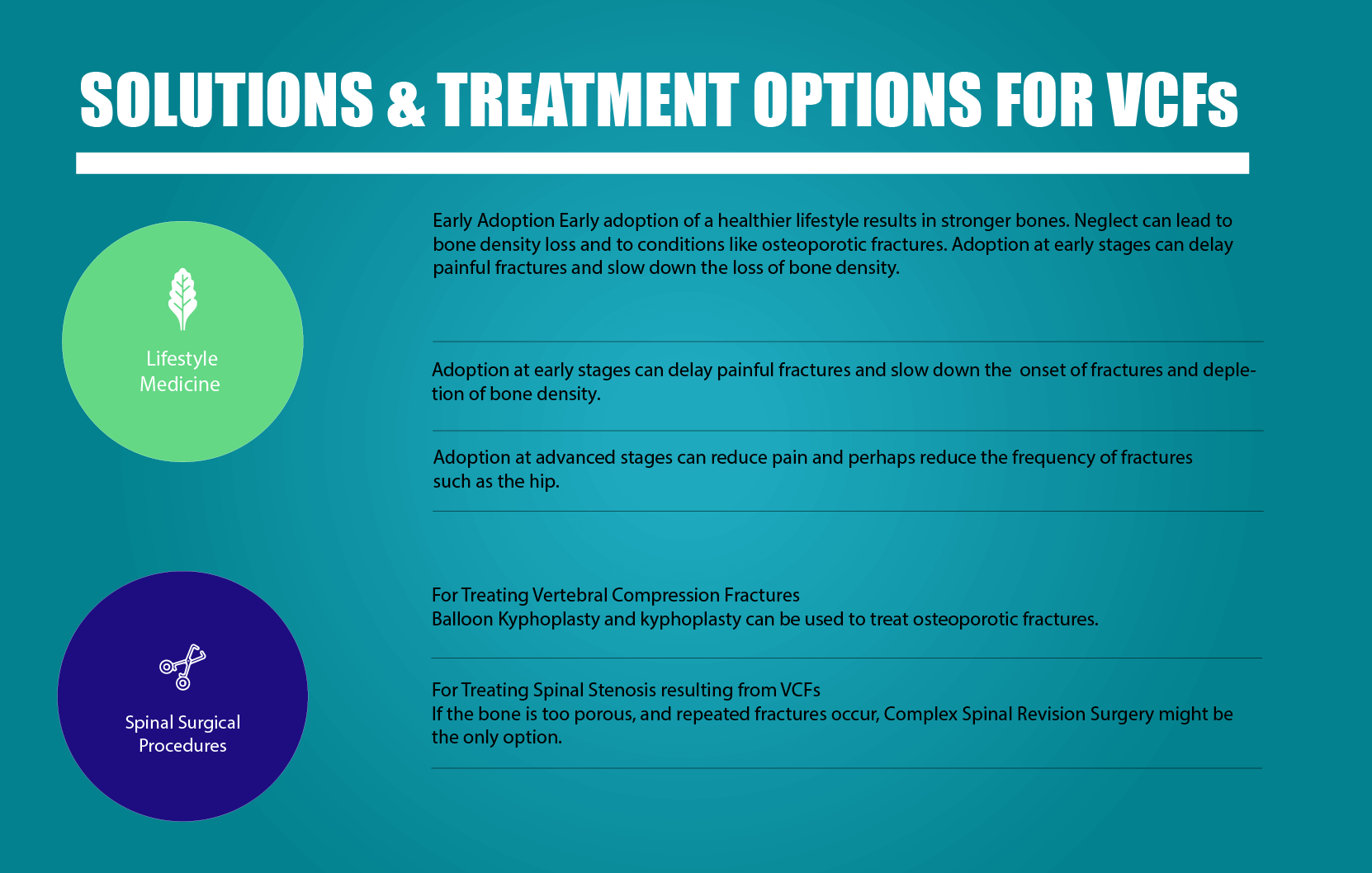
VCF-related pain if allowed to heal naturally can last as long as three months or more. However, the pain usually significantly decreases in a matter of days or even weeks. People with severe pain from VCFs are often recommended a reduction in strenuous activities, which would spark more pain. Rest and over-the-counter pain killers are also effective. Paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) are quite effective, as are muscle relaxants. Medicines for nerve/bone pain are often prescribed. Opioids, due to their addictive nature should be used for short periods of time (1-2 weeks) for acute pain, if at all. Back braces are sometimes used as external support and to limit the range of motion of the fractured vertebrae, like the support a cast provides on a leg fracture, but these are not generally tolerated by older people. Though immediate treatment is essential to alleviate the pain and the risks of fracture, the prevention of subsequent fractures is even more important. Your doctor may need to prescribe drugs known as bisphosphonates (i.e.: Actonel, Bonviva and Fosamax) to help stabilize or restrict bone loss. Also, additionally changes to lifestyle can help in ensuring that your spinal health improves naturally as well.
(b) Surgery
When conservative treatment options prove ineffective, a minimally invasive surgical procedure called balloon kyphoplasty, may be considered as a treatment option. Advances in spinal surgery have reduced the need for more risky invasive surgery in many cases. You can book a consultation with me. Telephone the hospital where you wish to see me, to book your appointment with me.
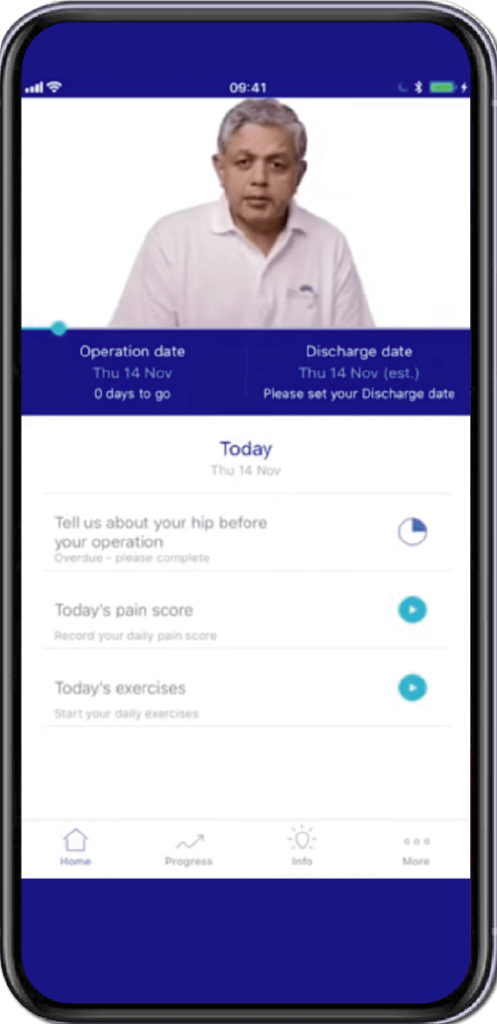
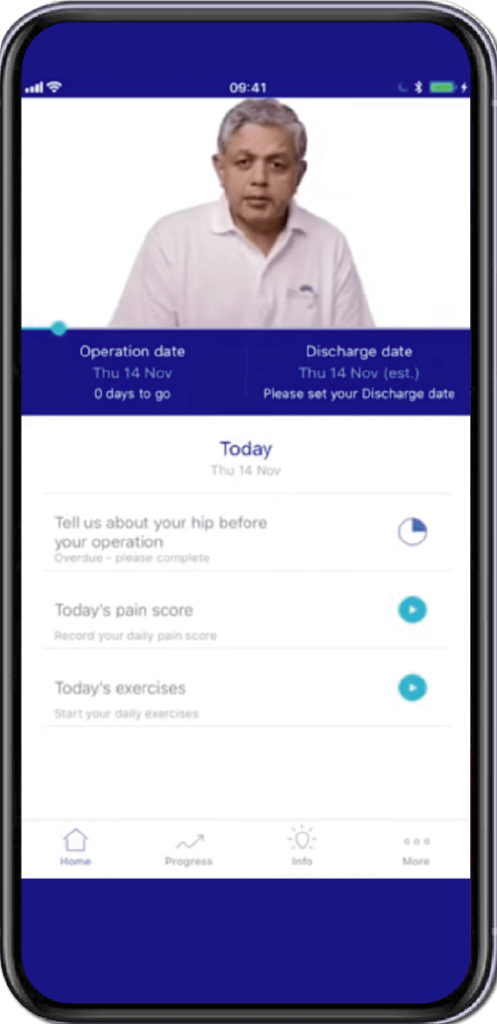
Specially Customised for you
Your version of the app will be customised specifically for you, by your surgeon.
This app will provide you with video messages from your consultant, highlighting key points during your patient journey.
To aid in your recovery process, it will provide you with:
- Interactive exercise plans
- Demonstration videos
- Progress graphs
- Useful articles chosen by your clinical team and more.
This app is in conjunction with Total Orthopaedics. To download the app, please scan in the QR code below:






Rajiv Bajekal is a Consultant Orthopaedic Surgeon with special interest in Spinal and Back-related issues. He has developed a pragmatic approach to managing back pain and sciatica with non-surgical techniques, injections and minimally invasive techniques. Mr Bajekal is also a Board-Certified Lifestyle Medicine Practitioner and believes in providing lifestyle medicine advice to his patients for better long term health gains and better spinal health. He has been consulting since 1998. He consults both privately and on the National Health Service (NHS) and is passionate about making sure patients are in control of their healthcare.
Mr Bajekal is a member of the following institutions:
- British Medical Association (BMA)
- British Association of Spine Surgeons
- British Society of Lifestyle Medicine (BSLM)
- Plant-Based Health Professionals
- Patient Information
- Hospital Practices
- Spire Bushey Hospital
- BMI The Cavell
- BMI The King’s Oak
- Contact
- Blog
- Resources
- Glossary
Additional Links
Mr Bajekal works in conjunction with Total Orthopaedics UK. For more details please click here.
For more detailed information on plant-based nutirition please visit: www.rohinibajekal.com
For more detailed information on women’s health please visit: www.nitubajekal.com
